What is CBD and how is it different from PSP & other tauopathies?
Introduction to Tauopathies
Tauopathies are a group of neurodegenerative diseases characterized by the abnormal aggregation of tau protein in the brain. Tau protein is the major neuronal microtubule-associated protein (MAP) encoded by the microtubule-associated protein (MAPT) gene, and promotes the assembly and stabilization of microtubules (Spillantini, 2013). While multiple diseases share this key feature of abnormal tau, they differ in how tau accumulates, the regions of the brain affected, and their clinical manifestations (Parmera, 2022). Tauopathies can be generally classified by tau pathology into three major groups as illustrated below (adapted from Ganguly, 2020). In this resource, we focus primarily on Corticobasal Degeneration (CBD) and how it compares to other tauopathies, such as Progressive Supranuclear Palsy (PSP).
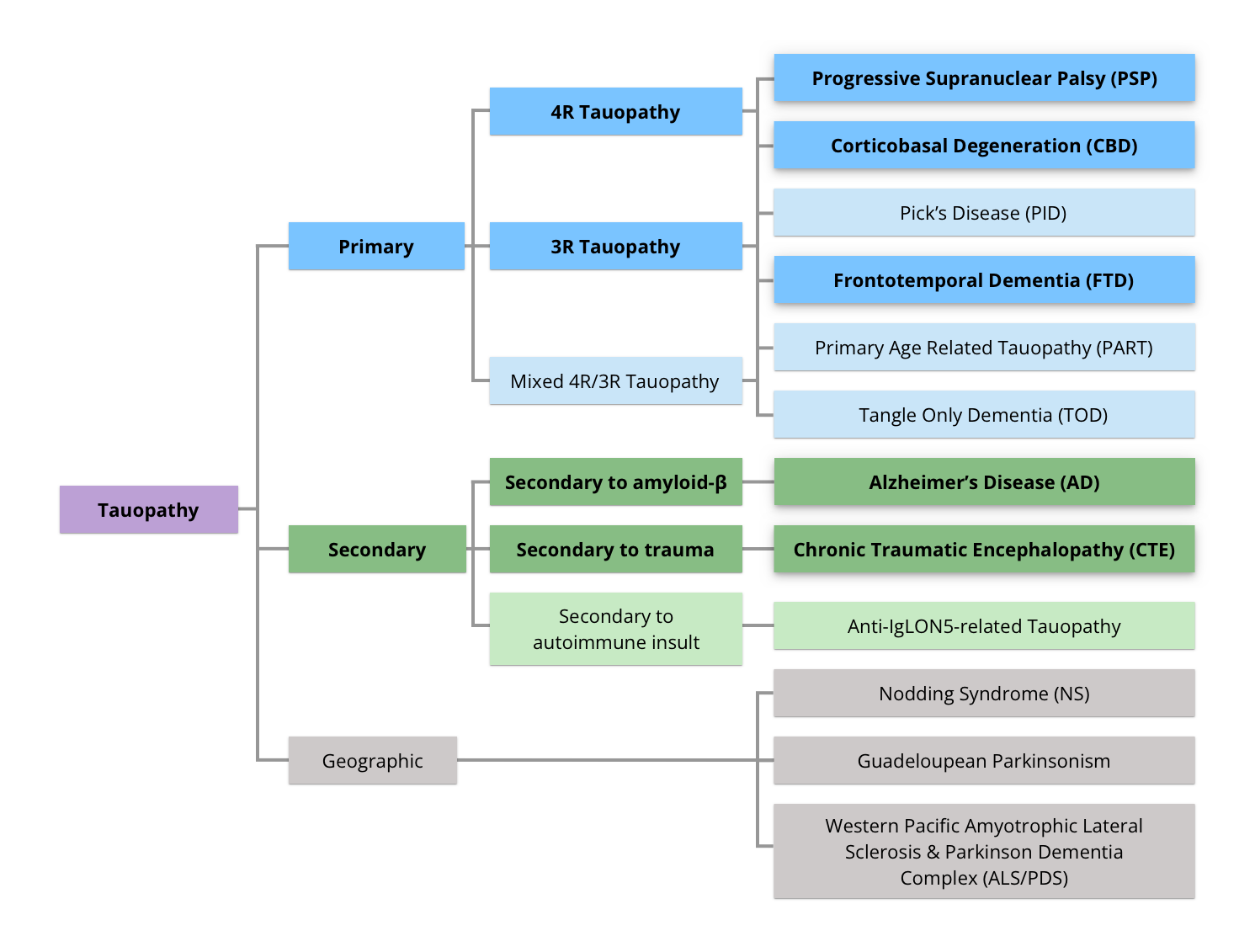
Hierarchical classification of tauopathies, divided into Primary, Secondary, and Geographic categories (figure derived from Ganguly, 2020, under the Creative Commons Attribution License).
Clinical Features and Diagnosis of CBD
CBD is a rare disorder that typically presents in the sixth decade of life, with a mean age of onset of 63.5 years, ranging from 45 to 77 years (Wenning, 1998; Josephs, 2006; (Ling, 2010). It affects men and women equally, often presenting with asymmetric motor disturbances (e.g. stiffness, slowness, and myoclonus) and cognitive impairment, such as aphasia, memory loss, and executive dysfunction. Other symptoms include dystonia, apraxia, and alien limb syndrome (Grijalvo-Perez, 2014). Due to the clinical overlap with other disorders, such as PSP and Parkinson’s disease (PD), as well as the lack of specific pre-mortem diagnostic markers, diagnosing CBD remains a challenge (Litvan, 1997).
Brain Regions Affected in CBD and PSP
The pathologic differences between CBD and PSP are primarily reflected in the distribution of tau protein in the brain. PSP involves more hindbrain pathology, whereas CBD shows more extensive cortical pathology (Dickson, 2002). PSP predominantly affects the brainstem, leading to symptoms such as postural instability, vertical gaze palsy, and neck stiffness. In contrast, CBD typically impacts the cortex and basal ganglia, presenting with more pronounced motor and cognitive asymmetries, including ideomotor apraxia and alien limb phenomena (Armstrong, 2013).
Cellular and Molecular Differences: Tau Pathology in CBD and PSP
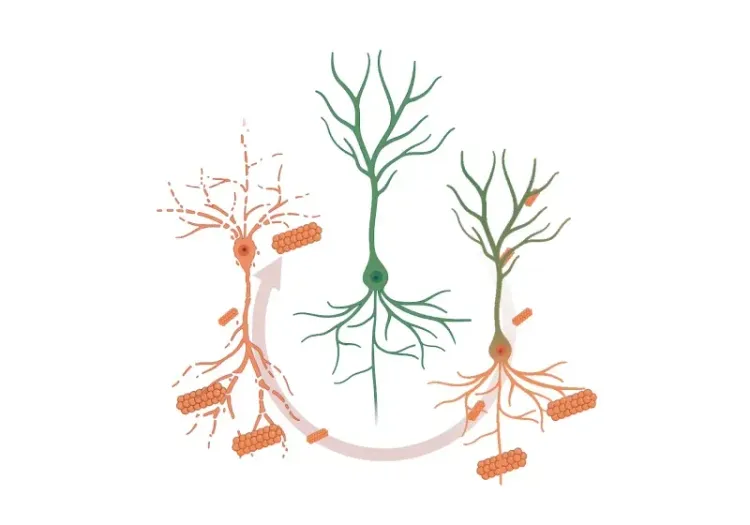
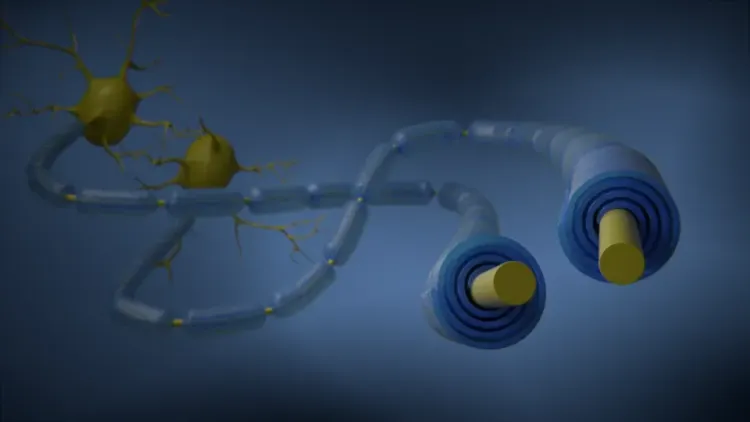
At the cellular level, both CBD and PSP are characterized by the deposition of abnormally hyperphosphorylated tau protein, particularly the four-repeat (4R) tau isoform (Constantinides, 2019). In both diseases, hyperphosphorylated tau loses its affinity for microtubules, resulting in microtubule dysfunction and a propensity for aggregation (Kouri, 2011). Immunoblotting of brain extracts shows different tau fragments in CBD and PSP, suggesting divergent proteolytic pathways contributing to their phenotypic differences (Arai, 2004).
Ballooned or achromatic neurons, once considered pathognomonic of CBD, are more commonly found in the cortical gray matter and less frequently in the basal ganglia (Rebeiz, 1967). However, recent research has identified astrocytic plaques as a defining feature of CBD, while tufted astrocytes are characteristic of PSP (Ferrer, 2014; Murray, 2014). Additionally, coiled bodies — tau deposits in oligodendrocytes — differ ultrastructurally between these diseases (Arima, 1997; Wakabayashi, 1994).
Comparison with Other Tauopathies: FTD, AD, and CTE
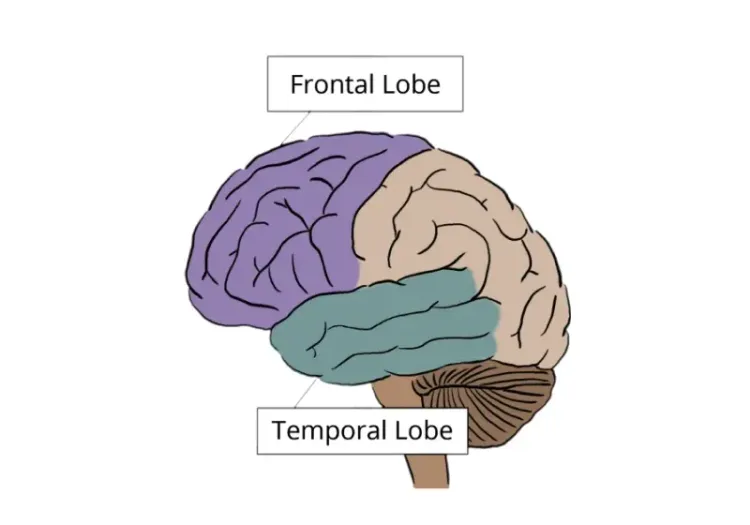
While CBD and PSP are distinct primary tauopathies, they share similarities with other tauopathies such as Frontotemporal Dementia (FTD), Alzheimer’s Disease (AD), and Chronic Traumatic Encephalopathy (CTE). FTD generally presents with early-onset dementia, affecting behavior and language more than motor functions. In contrast, CBD presents with more motor and cognitive impairments. FTD pathology can involve tau, TDP-43, and/or FUS proteins, predominantly affecting the frontal and temporal lobes (Mackenzie, 2010).
AD, the most common tauopathy, is marked by progressive memory loss and cognitive decline. Unlike CBD, where tau pathology is central, AD involves both amyloid-β plaques and neurofibrillary tangles in the hippocampus, cerebral cortex, and other brain regions (Jack, 2013). CTE, often associated with repetitive head trauma, can present with motor and cognitive symptoms similar to CBD or FTD. However, tau deposition in CTE occurs mainly in the depths of cortical sulci and perivascular regions, differing from the distribution in CBD (Tartaglia, 2014).
CBD, while sharing tau deposition with other tauopathies, such as PSP, FTD, and AD, presents distinct clinical and pathological features, particularly in its asymmetric motor and cognitive symptoms and its distribution of tau pathology in the cortex and basal ganglia. Differentiating these tauopathies requires careful analysis of clinical presentation, brain region involvement, and cellular-level tau pathology. Further research and development of biomarkers is needed for earlier diagnosis and better treatment strategies for these severe neurodegenerative diseases (Stamelou, 2021).
Which Imaging Biomarkers Can Be Used to Distinguish PSP and CBD?
There is a growing interest in developing disease-specific biomarkers to aid in predicting pathology for the antemortem diagnosis of neurodegenerative diseases. Tau pathology-targeted therapies are currently being developed in clinical trials (Höglinger, 2021). As such, there is a pressing need for diagnostic biomarkers capable of detecting PSP and CBD pathology in presymptomatic individuals or during the early phases of the disease. Advanced neuroimaging techniques have provided insights into the pathophysiological mechanisms and clinical symptoms associated with PSP and CBD (Parmera, 2022).
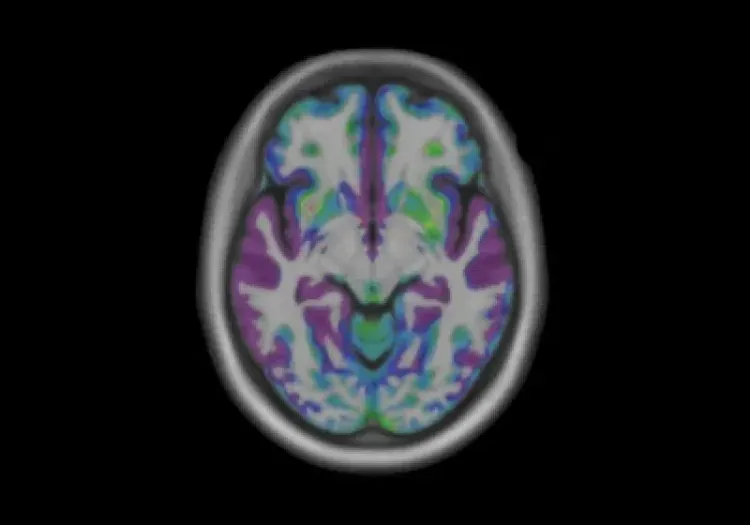
The primary imaging biomarkers that have been studied for PSP and CBD include structural imaging modalities, such as magnetic resonance imaging (MRI), and functional & molecular imaging using positron emission tomography (PET) and single-photon emission computed tomography (SPECT) (Parmera, 2022).
CBD typically presents with supratentorial patterns of atrophy, particularly asymmetrical patterns involving the posterior frontal lobe, superior parietal lobe, and basal ganglia. This pattern is often more pronounced in the hemisphere contralateral to the more affected limb. Additionally, motor severity has been found to negatively correlate with contralateral cortical thinning in the precentral and postcentral gyri and with volume of the putamen (Upadhyay, 2016).
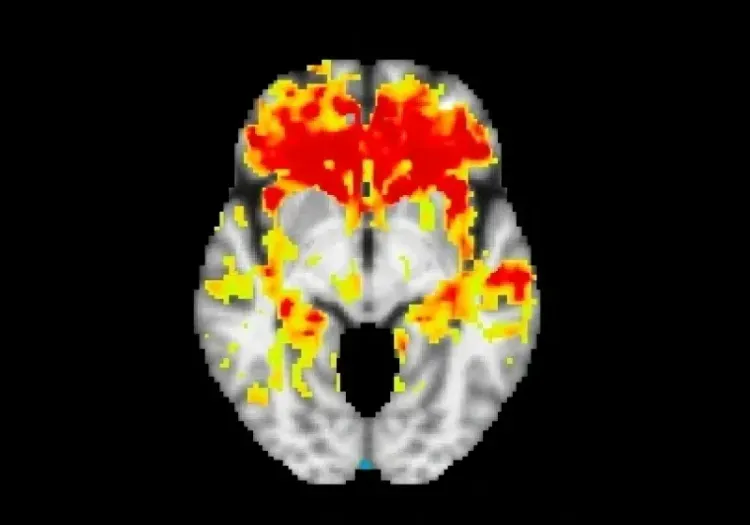
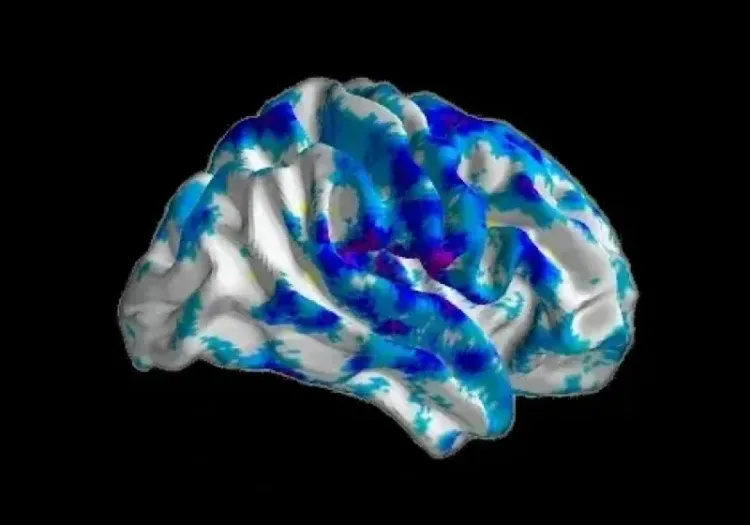
Multimodal MRI studies have been utilized to identify CBD patterns of structural alterations that may suggest underlying pathology. For example, a clinicopathologic study indicated that gray matter loss patterns in CBD differ based on the underlying pathology (Whitwell, 2010). Individuals with CBD who were later diagnosed postmortem with CBD or PSP displayed similar focal atrophy in premotor and supplementary motor areas. In contrast, patients with underlying FTD and AD pathology showed a more extensive pattern of gray matter loss in the frontotemporal and temporoparietal regions, respectively (Whitwell, 2010).
Changes in regional gray matter density over a period of 12 months in a CBD population. Statistically significant changes (FDR threshold = 0.05) in gray matter density are illustrated as statistical parametric maps overlaid on an anatomical MRI template. The deep purple and dark blue regions have the greatest loss of gray matter density.
Patients with CBD tend to present with asymmetric frontoparietal cortical atrophy, as well as thinning of the middle and posterior corpus callosum (CC) (Yamauchi, 1998; Dickson, 2002). A study comparing CBD to a PSP cohort characterized by severe midbrain and pons atrophy found that patients with CBD exhibited predominantly corpus callosum atrophy and mild midbrain atrophy. In this cohort, patients with CBD had decreased CC surface areas compared to other groups (such as PSP and MSA). A corpus callosum surface area below 470 mm² was highly specific (95%) for CBD, although it lacked sensitivity (67%) (Constantinides, 2018).
Another study, using voxel-based analysis, compared patterns of gray and white matter atrophy derived from MRI scans in autopsy-confirmed cases of PSP and CBD. It found that CBD showed more significant cortical gray matter atrophy, particularly in the posterior frontal and parietal regions and the basal ganglia (notably the putamen and pallidum) (Josephs, 2008). They also noted a marked difference between PSP and CBD in the lack of brainstem atrophy in CBD (Josephs, 2008).
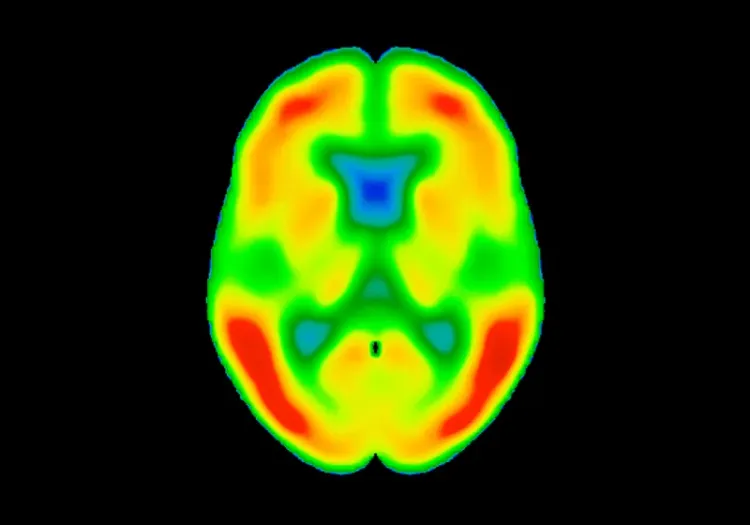
[18F]FDG PET has been shown to identify metabolic patterns linked to CBD, which often presents with asymmetric frontoparietal hypometabolism (Niethammer, 2014). It enhances diagnostic accuracy by distinguishing CBD from other conditions, such as AD, which shows more posterior temporoparietal hypometabolism (Pardini, 2019; Parmera, 2021). This ability to detect distinct metabolic signatures improves specificity for diagnosing CBD and related disorders.
Recent studies have enhanced our ability to distinguish PSP from CBD using neuroimaging biomarkers. Structural imaging, particularly MRI, reveals that CBD is typically marked by asymmetric atrophy in the frontoparietal regions and thinning of the corpus callosum, while PSP shows more severe atrophy in the midbrain and pons. Voxel-based analysis supports these findings by highlighting extensive cortical gray matter atrophy in CBD, in contrast to PSP's significant brainstem atrophy.
While these imaging techniques offer valuable insights, further research is needed to improve their accuracy and reliability. Developing non-invasive diagnostic tools for early detection remains a priority to reduce dependence on post-mortem confirmation.
How is MRS used to evaluate CBD?
Magnetic Resonance Spectroscopy (MRS), specifically proton (1H) MRS, is a non-invasive imaging technique that provides insights into the biochemical changes occurring in the brain. In the context of evaluating CBD, MRS is primarily used to measure the concentrations of key metabolites, which are indicative of neuronal health and integrity. The metabolites of interest in MRS are:
- N-Acetyl Aspartate (NAA): Predominantly found in neurons, NAA is considered a marker of neuronal and axonal density. Reduced levels of NAA suggest neuronal loss or dysfunction, which is a hallmark of neurodegenerative diseases, such as CBD (Ross, 2004).
- Choline (Cho): Choline is mainly associated with cell membrane constituents and is involved in the synthesis and degradation of phospholipids. Elevated levels of choline can indicate increased membrane turnover, which may result from neurodegenerative processes or inflammation (Buonocore, 2015).
- Creatine (Cre): Creatine and phosphocreatine are involved in energy metabolism. Typically, creatine levels are stable and often used as an internal reference in MRS studies. However, creatine levels can fluctuate under certain pathological conditions (Provencher, 2001).
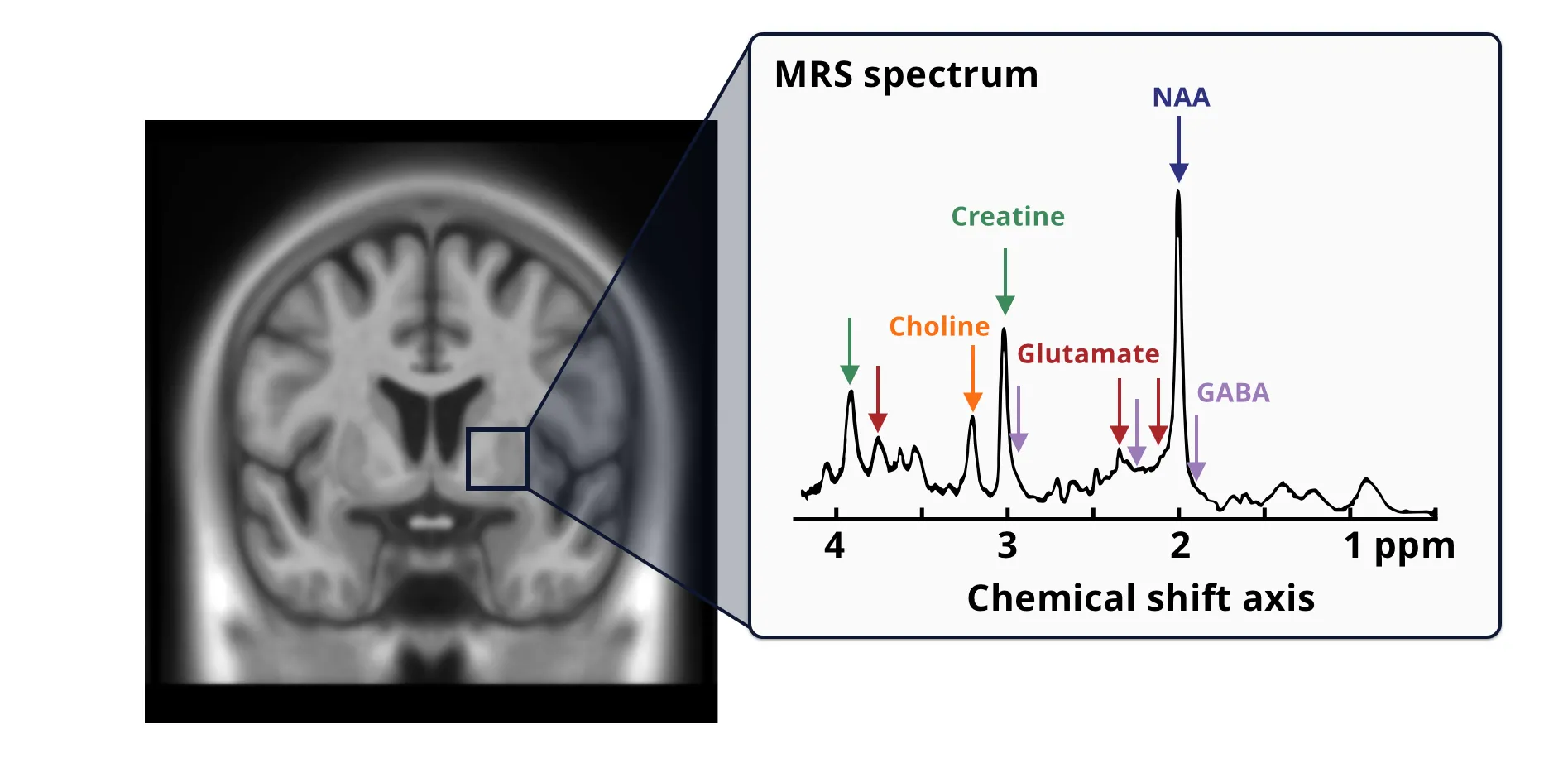
Metabolite signals are acquired using an 1H-MRS spectrum from a volume-of-interest (VOI, blue box). The MRS spectrum reflects the composite signal across all tissue types and cellular compartments within the VOI. Metabolites are identified using prior knowledge of their chemical properties and fitting the peaks along the chemical shift axis against known standards; quantities are measured in parts per million (ppm). Metabolite peaks are identified (from left to right) as belonging to choline (orange), creatine (teal), glutamate (red), N-acetyl aspartate (NAA, blue), and inhibitory neurotransmitter γ-aminobutyric acid (GABA, black). Multiple arrows of the same color indicate the multiple peaks that are associated with the same metabolite. The graph in the figure is derived from Figure 1 of Ip et al., 2022 under the Creative Commons Attribution License.
Research involving MRS in patients with CBD has demonstrated specific patterns of metabolite alterations:
- Decreased NAA/Creatine (NAA/Cre) and NAA/Choline (NAA/Cho) ratios have been consistently reported across studies. These changes are particularly observed in regions such as the basal ganglia, frontal cortex, centrum semiovale, parietal cortex, and perisylvian cortex. The basal ganglia is a common region-of-interest included in all studies, reflecting its relevance in CBD pathology (Tedeschi, 1997; Abe, 2000; Kizu, 2002).
- Two studies reported decreased NAA/Cre in the frontal cortex, while the parietal cortex and perisylvian regions also showed metabolite alterations. The asymmetry of these changes, particularly in the parietal cortex, helps differentiate CBD from other neurodegenerative disorders, such as Progressive Supranuclear Palsy (PSP), Multiple System Atrophy (MSA), and Frontotemporal Dementia (FTD) (Tedeschi, 1997; Abe, 2000).
In comparisons involving Parkinson's disease, PSP, and CBD:
- CBD patients exhibited significantly reduced NAA/Cre in the centrum semiovale and NAA/Cho in the lentiform nucleus and parietal cortex, especially contralateral to the most affected side. This observation suggests that MRS can detect specific patterns of neuronal loss and membrane turnover in these regions, potentially aiding in differentiating CBD from other disorders (Tedeschi, 1997).
- No significant differences were found between PD patients and control subjects regarding these metabolite ratios, suggesting that MRS may be more useful in distinguishing CBD from PD and PSP.
While MRS provides valuable data on regional brain metabolism and neuronal health in CBD, the ability to differentiate individual patients using 1H-MRS remains limited. However, the technique's capacity to detect distinct patterns of cortical and subcortical involvement supports its role in the diagnostic evaluation of CBD and potentially other neurodegenerative diseases.
Our team would be happy to answer any questions about Imaging Biomarkers to distinguish CBD from Other Tauopathies or provide specific information about our other Imaging services.
Discover more about our Imaging Services
Related Content
Up-to-date information on best practices related to the use of neuroimaging in clinical trials of neurological diseases.
Modeling Protein Misfolding in Neurological Diseases
Computational modeling of protein misfolding mechanisms in neurodegeneration and the application to discovery & development of disease-modifying therapeutics.
Diffusion MRI & Frontotemporal Dementia (FTD)
Diffusion neuroimaging analysis from the FTLDNI natural history study of Frontotemporal Dementia (FTD).
Frontotemporal Dementia (FTD) & MRI Brain Atrophy
Neuroimaging biomarkers (including MRI brain atrophy) from the FTLDNI natural history study of Frontotemporal Dementia (FTD).
MRI & Corticobasal Degeneration (CBD)
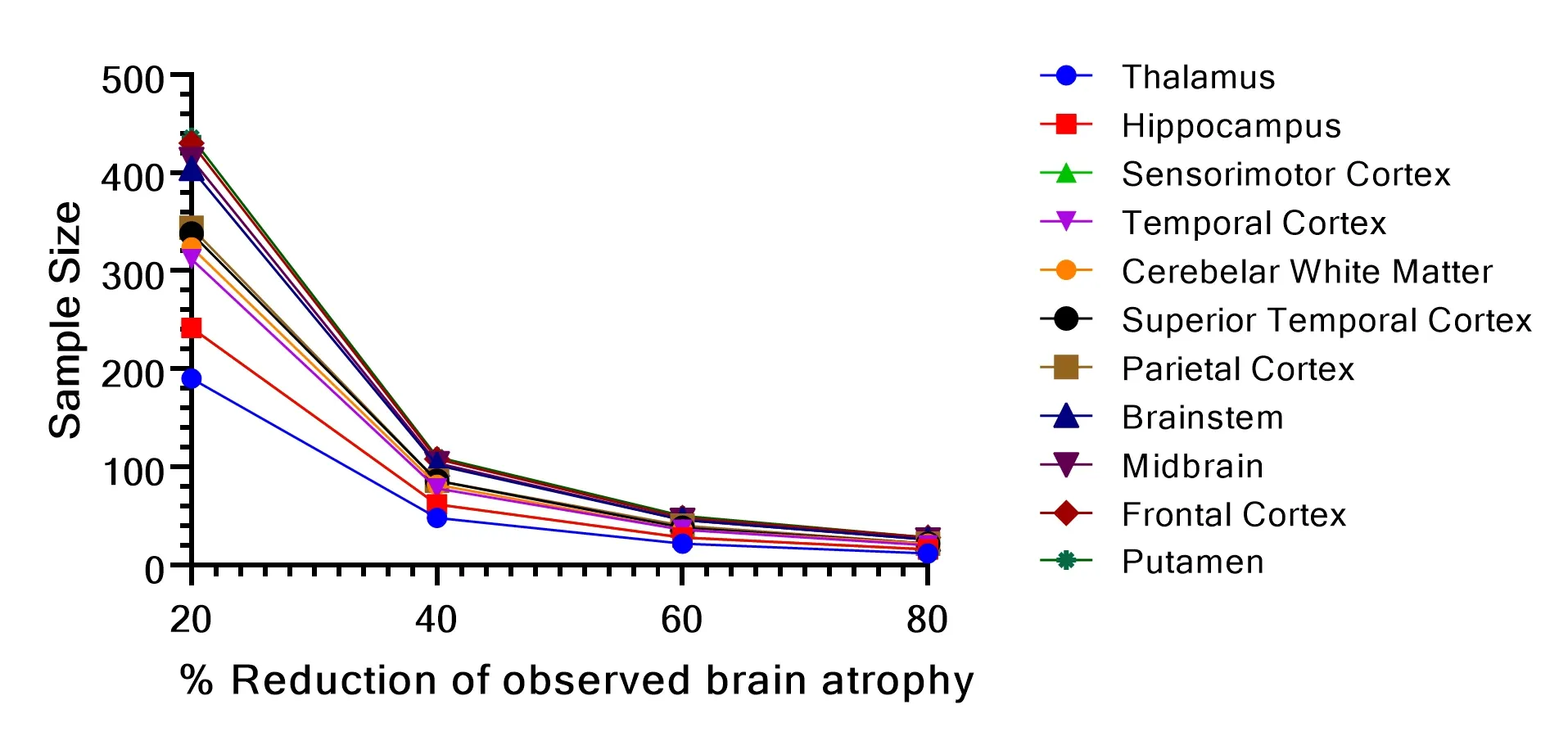
Longitudinal MRI brain atrophy measures from the 4RTNI and FTLDNI studies including sample size calculations for clinical trials of Corticobasal Degeneration.
Neuroimaging in Frontotemporal Dementia & Clinical Trials
The utility of MRI & PET imaging biomarkers in our understanding of Frontotemporal Dementia (FTD) variants, and their use as endpoints in FTD clinical trials.
MRI Gadolinium-Enhancing Lesions in MS Clinical Trials
How gadolinium (Gd) enhancing lesions are used to track disease progression & response to therapeutic intervention in multiple sclerosis (MS) clinical trials.
Imaging Biomarkers for Progressive Supranuclear Palsy (PSP)
An overview of the various brain imaging methods (MRI, PET, SPECT) available to assess efficacy of disease-modifying therapeutics in clinical trials of PSP.
Longitudinal Change in Tau PET in MCI & Alzheimer’s Disease
An overview of the natural history of change in Tau PET tracer uptake & binding in Mild Cognitive Impairment (MCI) & Alzheimer’s disease (AD).
MRI in Clinical Trials of Multiple System Atrophy (MSA)
This resource provides an overview of the utility of volumetric MRI and diffusion-weighted imaging (DWI) as biomarkers in research studies of MSA.