What are the clinical features and genetic underpinnings of FRDA?
Clinical Features
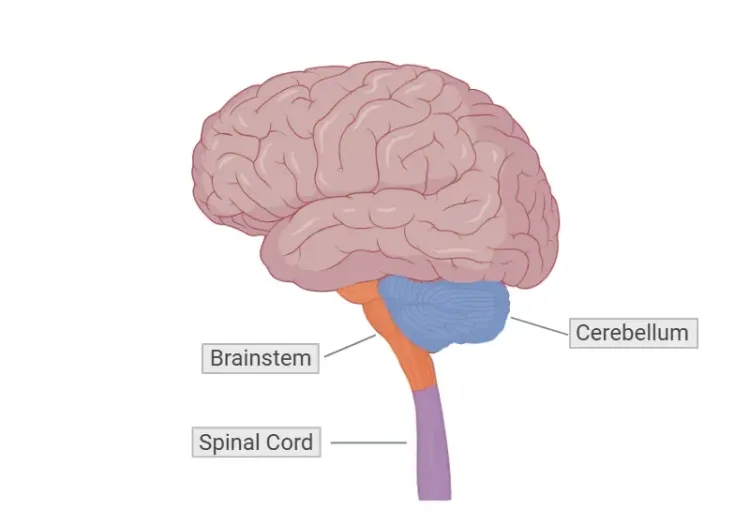
Friedreich’s ataxia (FRDA) is a rare, autosomal recessive neurodegenerative disorder characterized by progressive limb and gait ataxia, primarily affecting the spinal cord, cerebellum, and brainstem. FRDA is the most common autosomal recessive ataxia, with a prevalence of approximately 1 in 40,000 individuals, predominantly affecting those of Western and Southern European descent (Vankan, 2013). The disease typically presents in childhood or adolescence, usually between the ages of 10 and 15, although some children may show symptoms under the age of 10 (Bidichandani, 1998; Mahale, 2024). Less common forms include late-onset Friedreich’s ataxia (LOFA), presenting after age 25, and very late-onset (VLOFA), which appears after age 40 (Bidichandani, 1998). Both males and females are equally affected.
The clinical features of FRDA include progressive limb and gait ataxia, loss of coordination, and dysarthria, all of which are primarily neurological symptoms involving the brain and spinal cord. Additional neurological symptoms may include abnormal eye movements, hearing loss, and tremors (Pandolfo, 2009). Scoliosis is common, affecting a significant proportion of individuals with FRDA, and is considered a skeletal manifestation due to its association with muscle weakness and ataxia. Diabetes, a less common feature, often develops due to pancreatic involvement (Bidichandani, 1998). Cardiac involvement, particularly cardiomyopathy, is a severe feature of the disease, often leading to premature mortality. The disease course typically involves a gradual decline in mobility, with most individuals requiring wheelchair assistance approximately 10 years after symptom onset (Pandolfo, 2009).
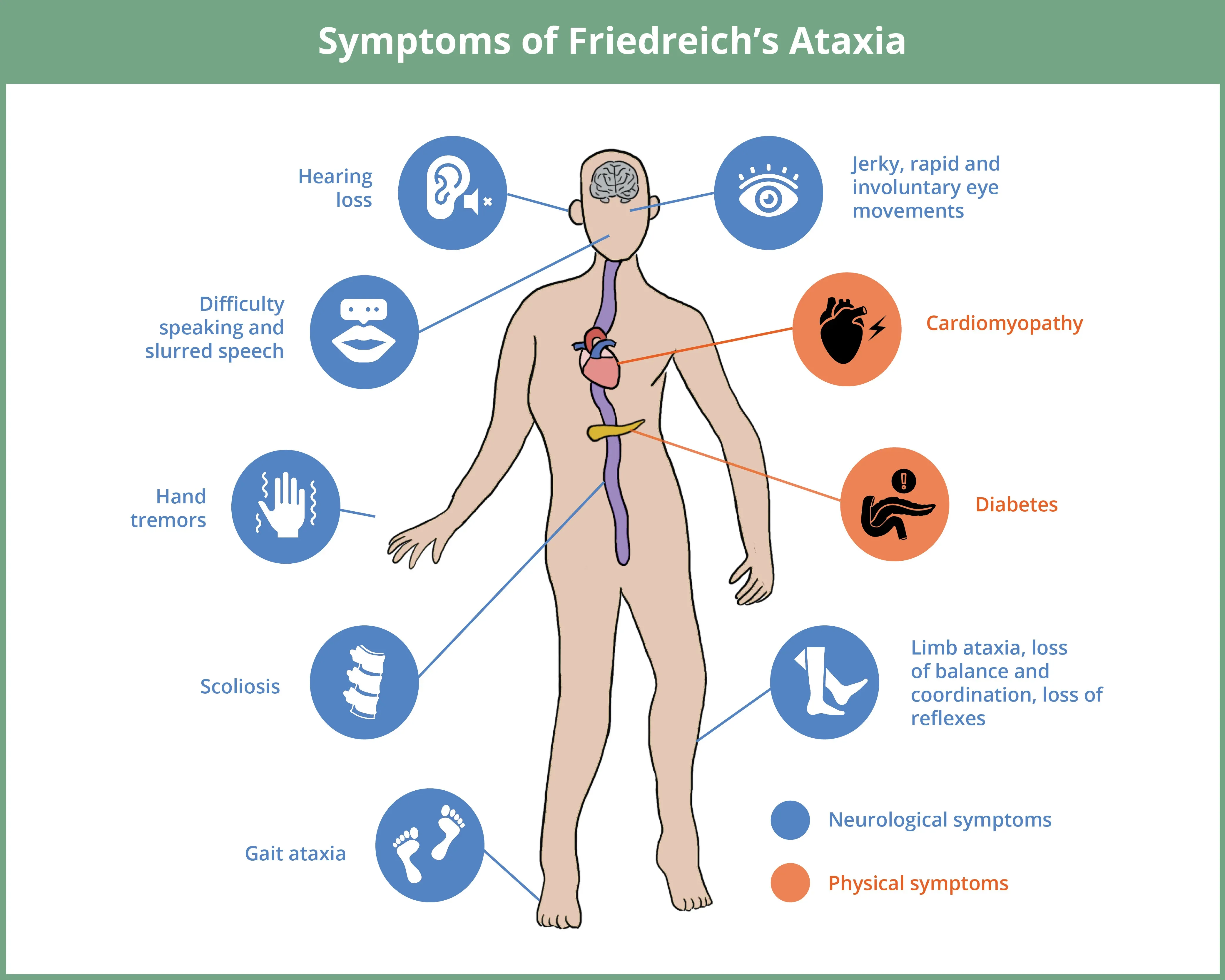
Friedreich’s ataxia (FRDA) is a rare neurodegenerative disorder that typically presents in childhood or adolescence, primarily affecting the spinal cord, cerebellum, and brainstem causing a range of neurological and physical symptoms.
Click to copy link
Genetic Underpinnings
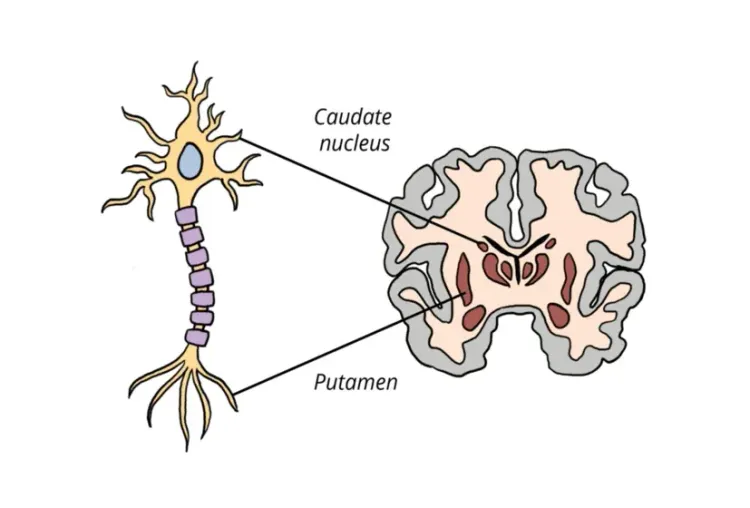
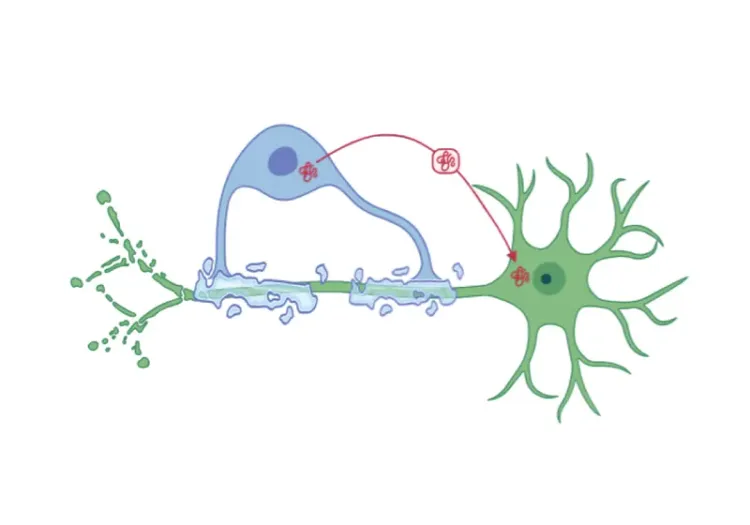
FRDA is caused by mutations in the FXN gene located on chromosome 9. The most common mutation is an expansion of GAA trinucleotide repeats in intron 1 of the FXN gene, leading to reduced production of the frataxin protein (Koeppen, 2011). Frataxin plays a critical role in mitochondrial function, particularly in iron regulation, and its deficiency results in oxidative stress and disrupted cellular metabolism (Dong, 2024). Approximately 96% of FRDA cases are caused by GAA repeat expansions on both alleles of the FXN gene, leading to significantly reduced levels of frataxin (Bidichandani, 1998). Research shows that the length of the GAA repeat expansion correlates with both earlier age of onset and increased disease severity (Pandolfo, 2009; Koeppen, 2011).
Heterozygous carriers of an FXN mutation show reduced frataxin levels but do not exhibit symptoms of FRDA. A smaller subset of cases (approximately 4%) involves one allele with a GAA repeat expansion and the other allele carrying a different mutation, such as a deletion or point mutation (Bidichandani, 1998). These cases tend to have milder clinical symptoms compared to those with two expanded alleles.
Diagnosis
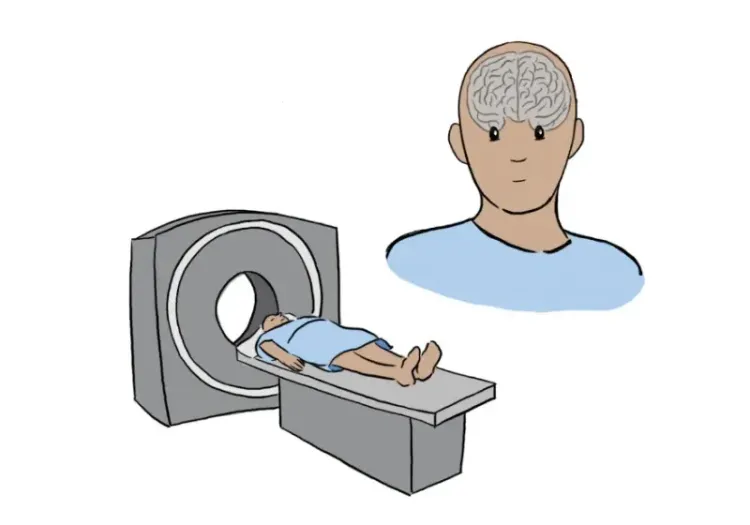
The diagnosis of FRDA is primarily based on clinical evaluation, which includes a physical examination to assess signs of ataxia, balance impairment, muscle weakness, and other neurological deficits (Bidichandani, 1998). Genetic testing to identify mutations in the FXN gene is used to confirm diagnosis, while echocardiography helps assess cardiac involvement. Neuroimaging techniques, such as magnetic resonance imaging (MRI) scans of the brain and spinal cord, are used to evaluate structural changes (Bidichandani, 1998).
Given the severe and complex nature of FRDA’s clinical features, there is a need for continued research into therapeutic interventions. Equally critical is the development of reliable biomarkers for early disease detection, which would enable timely interventions. The advancement of biomarkers, including imaging markers, is also essential for tracking disease progression and assessing the efficacy of therapeutic treatments in clinical trials.
What are the therapeutic targets in current clinical trials of FRDA?
Current clinical trials in FRDA focus on improving mitochondrial function, reducing oxidative stress, and modulating frataxin-controlled metabolic pathways. Other key areas of investigation include frataxin replacement therapies and gene replacement approaches.
Omaveloxolone (SKYCLARYS®), developed by Biogen, is the only FDA-approved treatment for FRDA, having received approval in February 2023, followed by approval by the European Commission in February 2024 (Pilotto, 2024). Several other companies and research institutions are advancing clinical trials for additional therapies. Notably, PTC Therapeutics is conducting a Phase 3 trial of vatiquinone (NCT05515536) (Lee, 2024). A Phase 1/2 trial of elamipretide, developed by the Children’s Hospital of Philadelphia and Stealth Biotherapeutics, is also underway (NCT05168774). Dimethyl fumarate is being tested in a Phase 2 trial in Italy (EUTC: 2022-503016-16-00). Larimar Therapeutics is exploring namlabofusp, a frataxin replacement therapy, in both Phase 1 (NCT06681766) a Phase 2 trials (NCT06447025) (Clayton, 2024). Gene replacement therapies are under investigation, including LX2006 by Lexeo Therapeutics in collaboration with Weill Cornell, which is in a Phase 1/2 trial (NCT05445323).
Additionally, the Friedreich’s Ataxia Research Alliance (FARA) has launched a significant natural history study, called TRACK-FA (NCT04349514), to investigate neuroimaging biomarkers in FRDA (Georgiou-Karistianis, 2022). The study, including over 200 FRDA participants across seven international sites, uses MRI, diffusion tensor imaging (DTI), and magnetic resonance spectroscopy (MRS) to explore longitudinal changes in key regions-of-interest, including the dentate nucleus, cerebellum, superior cerebellar peduncles, and spinal cord, at baseline, 12 months, and 24 months. The findings aim to identify imaging biomarkers that can track disease progression and serve as reliable endpoints in clinical trials.
Which MRI and DTI biomarkers are effective for detecting and tracking disease progression in FRDA?
FRDA primarily affects the cerebellum, spinal cord, and brainstem, with significant neuropathology in the dentate nucleus, dorsal root ganglia, and the spinocerebellar and corticospinal tracts (Harding, 2021). Widespread loss of brain white matter has also been observed (Harding, 2021). These pathologic changes are thought to result from both abnormal development and progressive degeneration (Rezende, 2023).
MRI is a key imaging technique in tracking disease progression in FRDA. It shows volume loss in cerebellar white matter, including the dentate nucleus, as well as other regions, such as the thalamus, pons, medulla, midbrain, and superior cerebellar peduncles (Adanyeguh, 2023). Longitudinal MRI studies demonstrate progressive atrophy, particularly in the cerebellum, thalamus, ventral diencephalon, pons, and midbrain (Adanyeguh, 2023). In contrast, the fourth ventricle has been shown to increase in volume as these regions atrophy.
DTI has revealed microstructural changes, particularly in the cerebellum and corticospinal tract (Adanyeguh, 2023). Longitudinal DTI analysis shows decreased fractional anisotropy (FA) and increased radial diffusivity (RD) in the superior cerebellar peduncles, along with an annual increase in RD in the inferior cerebellar peduncles (Adanyeguh, 2023). Degeneration of the dentato-thalamo-cortical tract (DTT) has also been observed, with decreased FA and increased mean diffusivity (MD) and RD, as well as significant correlations between GAA repeat length and DTI metrics, indicating that longer repeats are associated with more severe degeneration (Cocozza, 2024).
MRS has been employed to detect neurochemical changes in the cerebellum and spinal cord of FRDA patients. MRS studies have revealed alterations in metabolites, such as lower total N-acetylaspartate (tNAA) and higher myo-inositol (mIns) in the cerebellum, that are not visible with traditional imaging (Iltis, 2010). A study of the spinal cord showed lower tNAA and higher mIns in FRDA patients, leading to a decreased tNAA/mIns ratio compared to controls (Joers, 2022). Longitudinal data also demonstrated a 5.8% annual decrease in this ratio. Together, these results suggest neuronal loss, gliosis, and abnormal myelination in the brain and spinal cord of FRDA patients (Iltis, 2010; Joers, 2022).
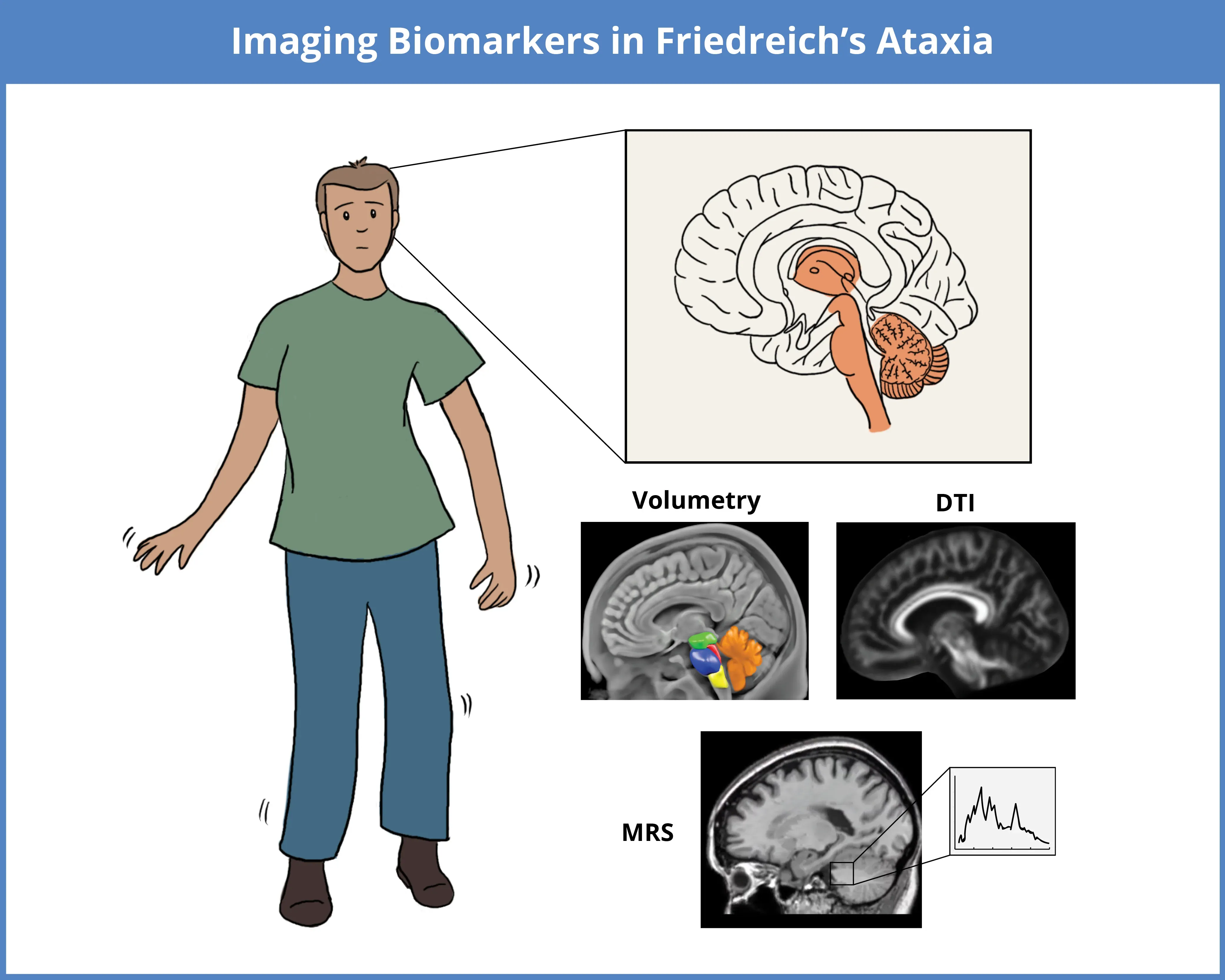
Imaging biomarkers used to assess FRDA include MRI-based structural volumetry for regional atrophy, DTI for microstructural changes, and MRS for neurochemical alterations. These techniques detect disease-related changes, particularly in the cerebellum, brainstem, thalamus, midbrain, and spinal cord.
MRI studies show that the extent of neuropathology in FRDA varies by disease stage (Harding, 2021). Volumetric MRI data suggest that changes in the dentate nucleus and brainstem occur early in the disease, while cerebral gray matter degeneration becomes more apparent in later stages (Harding, 2021). This volumetric MRI data corresponds with the clinical features of FRDA, where motor deficits predominate early, while cognitive, visual, and auditory symptoms may emerge later. Disease progression is influenced by GAA repeat length, with longer repeats linked to earlier onset and more severe disease progression. Volumetric studies indicate that an earlier age of onset is correlated with reduced white matter volume in the cerebellum, while decreased volumes in both the cerebellum and brainstem are negatively correlated with disease duration and severity (Harding, 2021).
In summary, MRI and DTI are the primary imaging modalities used for detecting and tracking disease progression in FRDA. These techniques provide reliable biomarkers for assessing structural and microstructural changes in key regions-of-interest, such as the dentate nucleus and spinal cord. In addition, MRS offers additional insights into neurochemical changes, detecting alterations in brain metabolites. Future multi-center clinical trials that incorporate various imaging modalities and stratify participants by various factors, such as age of onset and disease stage, will provide a more comprehensive understanding of FRDA and contribute to the development of new therapies.
Our team would be happy to answer any questions about Neuroimaging in Friedreich's Ataxia & Clinical Trials or provide specific information about our other Imaging services.
Discover more about our Imaging Services
Related Content
Up-to-date information on best practices related to the use of neuroimaging in clinical trials of neurological diseases.
Spinocerebellar Ataxia Clinical Trials & Imaging Biomarkers
An overview of structural MRI, DTI and MRS imaging biomarkers to monitor disease progression in spinocerebellar ataxia clinical trials.
PET Imaging in Huntington’s Disease Clinical Trials
An overview of the use of PET imaging biomarkers for Huntington’s disease (HD) clinical trials.
Neuroimaging Biomarkers for Tuberous Sclerosis Complex (TSC)
Overview of brain structural MRI and diffusion-weighted imaging biomarkers to monitor efficacy of disease-modifying therapeutics in clinical trials of TSC.
MRI Biomarkers in Clinical Trials of Huntington’s Disease
An overview of the use of structural and diffusion MRI imaging biomarkers for Huntington’s disease (HD) clinical trials.
Frontotemporal Dementia (FTD) & MRI Brain Atrophy
Neuroimaging biomarkers (including MRI brain atrophy) from the FTLDNI natural history study of Frontotemporal Dementia (FTD).
MRI in Clinical Trials of Multiple System Atrophy (MSA)
This resource provides an overview of the utility of volumetric MRI and diffusion-weighted imaging (DWI) as biomarkers in research studies of MSA.