What is [18F]DOPA?
[18F]DOPA (fluorodopa, also referred to as 18F-DOPA, [18F]F-DOPA, [18F]FDOPA, or, more formally, 6-[18F]fluoro-L-DOPA, 6-[18F]FDOPA, or 6-[18F]fluoro-L-3,4-dihydroxyphenylalanine) is a radiopharmaceutical tracer used in positron emission tomography (PET) imaging (Booij, 1999; Deng, 2002). It is a labeled form of L-DOPA, a precursor of dopamine (DA), a key neurotransmitter involved in movement, motivation, and reward.
The primary application of [18F]DOPA is to evaluate the function of dopaminergic systems in the brain. Several decades ago, in vivo [18F]DOPA PET tracer uptake was shown to reflect dopamine cell count levels following post-mortem brain examination (Snow, 1993). Since then, studies have consistently shown that declining [18F]DOPA uptake correlates with the loss of dopaminergic neurons in Parkinson’s disease (PD), particularly in the putamen (Morrish, 1996, 1998; Hilker, 2005; Maetzler, 2009; Nandhagopal, 2009; Arya, 2024). As such, it is widely regarded as a valuable imaging tool for the study of movement disorders, such as PD. Besides the application to PD and related movement disorders, [18F]DOPA is also used in studies of Huntington’s disease (Michler, 2019), as well as in oncological applications to visualize and assess tumors (e.g. glioma) (Breen, 2022). In addition, the use of [18F]DOPA PET is also being evaluated for other diseases, such as fibromyalgia (Ledermann, 2021).
[18F]DOPA was officially approved in the EU in 2006 and in the United States in 2019 for diagnosing PD and distinguishing essential tremor from Parkinsonian syndromes (Chevalme, 2007; Dhawan, 2020; Dhawan, 2022). This approval marked a significant milestone, broadening the scope of [18F]DOPA’s clinical application. Beyond its primary use in studying dopaminergic function, ongoing trials aim to improve image quality or expand their use in other populations and conditions (Abele, 2021). Additionally, studies are investigating the potential of [18F]DOPA PET imaging in managing psychiatric disorders, such as schizophrenia and mood disorders, due to its ability to map dopaminergic activity and dysfunction in the brain (Cheng, 2020).
What are the advantages and disadvantages of [18F]DOPA compared to other tracers, e.g. DaTscan?
Mechanism
First, to briefly summarize dopaminergic neurotransmission: dopamine is synthesized by the conversion of L-Tyrosine by tyrosine hydroxylase (TH) to L-DOPA followed by decarboxylation of L-DOPA by aromatic L-amino acid decarboxylase (AADC) (Meiser, 2013). It is then stored in synaptic vesicles and released into the synaptic cleft for signal transduction via the D2 receptor. The dopamine transporter (DAT) pump facilitates the reuptake of dopamine from the synaptic cleft back into the presynaptic neuron, and the vesicular monoamine transporter (VMAT2) then loads dopamine into the synaptic vesicles again. Different molecular imaging tracers target (bind to) different molecules along the dopaminergic neurotransmission pathway, as illustrated in the figure.
Nerve terminal illustrating the various radiotracers used to study the dopaminergic system. [18F]DOPA is decarboxylated to [18F]DA ([18F]dopamine) and stored in synaptic vesicles. VMAT-2 (vesicular monoamine transporter type 2) is labeled by [11C]DTBZ or [18F]DTBZ, and the dopamine transporter (DAT) is labeled by [11C]MP (PET) or [123I]FP-CIT (DaTscan SPECT). Dopamine D2/3 receptor availability can be labeled by [11C]RAC (raclopride), which is sensitive to synaptic levels of dopamine.
[18F]DOPA primarily reflects dopamine synthesis and storage, and thus provides information about presynaptic dopaminergic function (Morrish, 1996; Heiss, 2004); whereas [123I]FP-CIT (the tracer used for DaTscan SPECT) binds to the dopamine transporter (DAT) and thus reflects the integrity and density of the presynaptic dopamine terminals, not synthesis (Booij, 1999; Seppi, 2006; Kägi, 2010). Which of these tracers is used in any specific study depends on several factors, such as the specific hypothesis for and mechanism of action of, a drug candidate, the expected specificity and sensitivity of the tracer to drug-induced changes, and other study design considerations (Bidesi, 2021).
Other common PET tracers targeting the same processes include 11C-DTBZ ([11C]dihydrotetrabenazine) and 18F-DTBZ ([18F]DTBZ, commonly known as AV-133 or florbenazine) that both bind to the vesicular monoamine transporter 2 (VMAT2), responsible for packaging neurotransmitters like dopamine into presynaptic vesicles (Stoessl, 2012; Marek, 2018); 11C-RAC ([11C]raclopride) that primarily binds to postsynaptic dopamine receptors, often used to determine how drugs occupy D2/3 receptors (Volkow, 1994; Boileau, 2007); and 11C-MP ([11C]methylphenidate), a DAT blocker that binds to DAT sites in the striatum (Morrish, 1998; Volkow, 2002; Nandhagopal, 2009).
Practical Applicability
DaTscan SPECT is widely used to study Parkinsonian syndromes due to its relatively low cost, broad regulatory approval, and general clinical applicability. The relatively long half-life of the [123I] tracer, which is approximately 13 hours, permits shipment to a wide geographic area, thereby aiding in the logistics of scanning patients in multi-center clinical trials. On the other end of the spectrum, the [11C] tracers used for 11C-DTBZ, 11C-RAC, and 11C-MP have a very short half-life (~20 minutes), which means that an on-site cyclotron is required for PET scanning using these tracers, a major practical obstacle for multi-center clinical trials. The half-life of fluorine-18, used for [18F]DOPA and [18F]DTBZ PET, is around 110 minutes, which is still relatively short compared to DaTscan, but allows for considerably more flexibility than [11C].
A major advantage of PET compared to DaTscan is the image spatial resolution. DaTscan SPECT has low image resolution, typically ~7-8mm, whereas PET scans can be acquired at spatial resolutions of ~4-5mm or even higher, which increases the anatomical specificity of the acquired images (Rahmim, 2008; Khalil, 2011). In addition, [18F]DOPA has the advantage of directly measuring dopamine synthesis through its uptake and conversion by AADC, which underpins its use in early detection. This property makes it an excellent choice for studying early PD and assessing the synthetic capacity of dopaminergic neurons. DaTscan SPECT, on the other hand, is primarily used for clinical diagnosis of PD, as well as differentiating PD from other movement disorders; [18F]DOPA PET is better suited to monitor disease progression and the assessment of treatment effect.
Additionally, [18F]DOPA also has a substantial logistical advantage over DaTscan SPECT, given that the scanning time is only 10-20 minutes, compared to 30-45 minutes for DaTscan; also, the post-injection time (time between injection of the tracer and the scanning session) is considerably shorter for [18F]DOPA PET (60-90 minutes compared to 3-6 hours). Especially for a patient population with movement disorders, reducing the preparation and scanning time can be of vital importance to image data quality.
The following table summarizes the different aspects of these tracers:

Summary of different features of radiotracers used for dopaminergic imaging.
In summary, even though DaTscan SPECT is widely used, [18F]DOPA PET is advantageous in clinical trials of movement disorders as it more directly measures dopamine synthesis, has higher sensitivity, offers considerably higher imaging spatial resolution, and has reduced scanning time. Limitations in this context are that it is more costly and does require a nearby cyclotron facility. The various [11C] tracers can be useful in focused, small-scale studies at dedicated research sites, but the high cost and requirement of an on-site cyclotron facility severely limit their applicability in larger, multi-center clinical trials.
Is [18F]DOPA PET an effective biomarker for monitoring disease progression in movement disorders?
General Overview
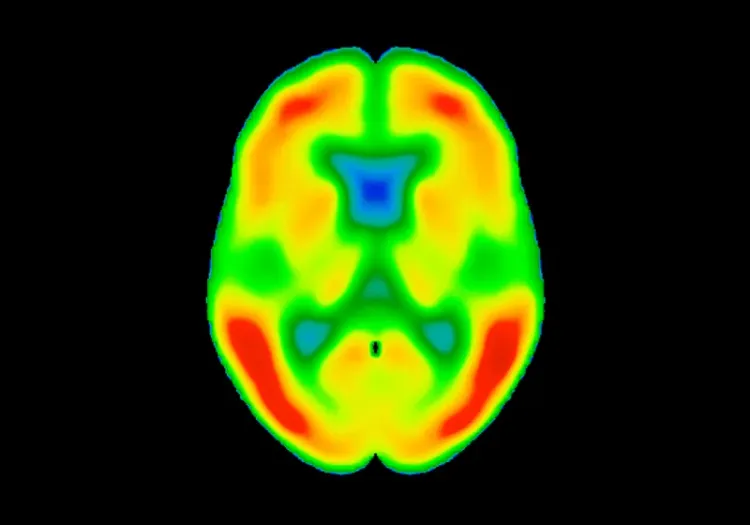
In typical PD, [18F]DOPA uptake in striatal regions decreases compared to healthy state and atypical Parkinson’s syndromes. During the clinical phase of the disease, repeated [18F]DOPA PET imaging in longitudinal studies has demonstrated a relatively consistent annual decrease in putamen tracer uptake—often in the range of 8–12% in early-to-moderate disease—which supports the efficacy of [18F]DOPA PET to quantify and track disease-related changes (Nandhagopal, 2009). The decrease is usually asymmetrical, with signal loss greater in one hemisphere of the brain (the side contralateral to the more affected limbs) as compared to the other hemisphere (Whone, 2003; Kuriakose, 2010). In addition, the posterior putamen is often more affected than the anterior putamen, and that gradient tends to be maintained throughout the course of the disease (Nandhagopal, 2009; Ibrahim, 2016).
Although most studies of the use of [18F]DOPA in PD have focused on striatal regions, specifically the putamen and caudate nucleus, there is also evidence that tracer uptake differentiating Parkinson’s patients from healthy controls can be detected in other brain regions, such as diencephalon, brainstem, and other cortical and subcortical regions, including the amygdala (Smith, 2008).
The decrease in striatal uptake of [18F]DOPA correlates with the severity of certain motor symptoms, especially rigidity and bradykinesia (Otsuka, 1996; Niethammer, 2012); However, [18F]DOPA uptake does not appear to correlate with all Parkinsonian disease symptoms. For example, non-motor symptoms such as cognitive impairment and depression, as well as some motor symptoms, such as tremors, do not correlate well, which suggests they may be caused by other factors beyond dopaminergic terminal degradation (Otsuka, 1996; Broussolle, 1999).
One key advantage of [18F]DOPA is its sensitivity to early changes in dopamine signaling in the striatum. Even before overt motor symptoms manifest, [18F]DOPA PET can detect subtle reductions in dopaminergic synthesis, potentially identifying individuals at higher risk of progression to clinically evident PD (Vingerhoets, 1994; Trujillo, 2025). In an older study, using [18F]DOPA uptake measurements in PD patients taken at two timepoints 18 months apart, the authors estimated that the average preclinical (asymptomatic) period of PD is likely no longer than 7 years (Morrish, 1998; Hilker, 2005). However, there are indications that the mechanisms underlying [18F]DOPA tracer uptake are probably different between disease initiation and progression, implying that evaluating disease-modifying strategies should take these differences into account in clinical trial settings (Nandhagopal, 2009). That same study, based on following 78 patients with 4- and 8-year follow-up scans, demonstrated an exponential decline in dopaminergic function, with the steepest decline in the first 5 years following symptom onset. The authors argue that in order to characterize that exponential decline, longitudinal data is essential and allows for an up to 5-fold decrease in sample size needed to estimate the parameters of the decline compared to cross-sectional data. A more recent meta-analysis (Kaasinen, 2017) reported similar findings.
Use of [18F]DOPA PET as a Biomarker in Clinical Trials
The goal of a biomarker in the study of disease-modifying therapies is ultimately to demonstrate that the therapeutic preserves or improves symptoms or clinical outcomes. A biomarker may qualify as a surrogate endpoint in a clinical trial if it (1) correlates with, or even anticipates clinical progression, and (2) shows superiority over clinical measurements in terms of practicability, precision, effect size, or any combination of these (van Eimeren, 2019). In terms of correlation with clinical progression, many studies have shown strong agreement between [18F]DOPA PET and the Unified Parkinson’s Disease Rating Scale (UPDRS) motor scores (Morrish, 1998; Pirker, 2003; Brooks, 2011; Kaasinen, 2017). This data underlines the potential of [18F]DOPA not only for diagnosis, but also for monitoring disease progression in movement disorders.
A number of manuscripts, meta-analyses, and position statements covering the potential utility of dopaminergic imaging, and specifically using [18F]DOPA as a biomarker, in clinical trials have been written over the years (Pirker, 2003; Maetzler, 2009; Nandhagopal, 2009; Niethammer, 2012; Kaasinen, 2017, 2019; Strafella, 2017; van Eimeren, 2019; Bidesi, 2021). In addition, the Parkinson’s Progression Markers Initiative (PPMI) (Marek, 2011, 2018; Simuni, 2018) is a long-running, large-scale research study that aims to address this and other questions relating to the course PD. Although these studies overall show agreement on the hallmarks of dopaminergic imaging in PD and related disorders, specifically striatal reduction of dopaminergic neurons, they also demonstrate considerable variability. The variability is thought to be due to several factors, such as (a) individual variability in the disease onset, staging, and progression, (b) variability inherent to scientific studies with small sample sizes, and (c) variability in the data acquisition methodology (Kaasinen, 2017).
However, as noted, the fairly strong decline of dopaminergic neurons in PD is well-described. For example, one paper reports an annual decrease of 8.1% in putamen and 6.3% in the caudate nucleus (Hilker, 2005), which is comparable to what other studies have found (Nurmi, 2001; Kaasinen, 2017). In contrast, the decline in healthy controls is reported to be less than 2.5% annually (Maetzler, 2009). The effect is even stronger in early PD, with reports showing at least 30% reduction in [18F]DOPA uptake in putamen, contralateral to clinical symptoms (Jokinen, 2009). These effect sizes are sufficiently large to be able to detect a treatment effect even with relatively small sample sizes; especially if the treatment effect results in restoration of dopaminergic function. For example, multiple studies of dopaminergic cell transplantation (Nakamura, 2001; Ma, 2010) have demonstrated substantial and significant increases in [18F]DOPA uptake in cohorts of 30-40 patients over a period of 1-4 years following the transplantation, reaching over 40% increase in uptake over a period of 4 years.
Determining the sample sizes needed to detect a treatment effect depends on a number of factors and assumptions, primarily the expected effect size, variability of the measurement, and the study design. In one study, the within-subject variability of striatal [18F]DOPA uptake measurements was been estimated to be in the range of 3-8% (depending on the exact anatomical region-of-interest [ROI]) within-subject, and 6-12% between-subject; while extra-striatal variabilities were higher, ranging from 8-20% between-subject and 6-20% within-subject, strongly dependent on the ROI (Egerton, 2010). The authors note that the relatively high variability in extra-striatal regions is likely due to the low signal-to-noise ratio in those areas. Note that this study was conducted under tightly controlled conditions, with uniform acquisitions all performed at a single site which would result in considerably less variability compared to a multi-site study. But to illustrate, assuming a target effect size of 10% and measurement variability of 10%, a placebo-controlled clinical trial would need at least 16 subjects in each arm to be able detect such a treatment effect (assuming 80% power and a significance level of 0.05). If the measurement variability, in reality, would be 20-40%, that sample size needed to detect the same treatment effect would increase to 63-142 subjects per arm, illustrating the importance of the reduction of variability in clinical trials as that translates directly to trial cost.
Comparing to DaTscan, the annual decline in DAT binding in the putamen has been reported to be similar to that assessed with [18F]DOPA PET (Benamer, 2000; Pirker, 2003); however, the measurement variability of DaTscan is higher due to the lower resolution, varying image reconstruction methods, and higher site-to-site variability, leading to 1.2-1.5 times more participants needed in a typical clinical trial (Seppi, 2006; Kägi, 2010; Brooks, 2011). Additionally, an important consideration comparing DaTscan SPECT to [18F]DOPA PET is also that due to the higher imaging resolution, PET offers better regional discrimination, in principle improving, for example, the ability to identify anterior-posterior gradient of the tracer uptake in the putamen or differential uptake between putamen and caudate nucleus (Khalil, 2011).
In summary, [18F]DOPA remains one of the most established PET tracers, and the de facto standard, for monitoring dopaminergic neuronal integrity in PD and related movement disorders, making it a valuable biomarker for disease progression when the necessary imaging infrastructure is in place or accessible (Tian, 2024). Additionally, [18F]DOPA PET is also increasingly considered for use in standard clinical practice (Walker, 2011).
However, while [18F]DOPA PET provides valuable information on dopamine synthesis, it does not directly measure other aspects of dopaminergic function, such as dopamine transporter density (as assessed by DaTscan or 11C-MP PET) or vesicular storage (as seen with DTBZ tracers). Thus, it may be most informative when used within a multimodal approach, potentially complementing other tracers or clinical assessments (Nandhagopal, 2009); and more sophisticated analysis techniques, such as deep learning (Zhao, 2022). The application of [18F]DOPA in large-scale, multi-center clinical trials requires reducing the various sources of variability as much as possible, through careful selection of patient population and standardization of acquisition and analysis protocols (Whone, 2004).
Our team would be happy to answer any questions about the Use of [18F]DOPA in Clinical Trials of Parkinson’s Disease or provide specific information about our other Imaging services.
Discover more about our Imaging Services
Related Content
Up-to-date information on best practices related to the use of neuroimaging in clinical trials of neurological diseases.
PET Imaging in Huntington’s Disease Clinical Trials
An overview of the use of PET imaging biomarkers for Huntington’s disease (HD) clinical trials.
Longitudinal Change in Tau PET in MCI & Alzheimer’s Disease
An overview of the natural history of change in Tau PET tracer uptake & binding in Mild Cognitive Impairment (MCI) & Alzheimer’s disease (AD).
Decreased Brain Glucose Metabolism in MCI is Driven by Tau
We demonstrate a more significant role of tau than β-amyloid in the reduction of cerebral glucose metabolism by analysis of PET images from the ADNI study.
Computational Method for Harmonization of Brain PET Images
A new algorithm for standardizing the spatial resolution of brain positron emission tomography (PET) images in multicenter clinical trials without phantoms.