Alzheimer's Disease Imaging in Clinical Trials Overview
Multi-modality imaging is widely used in early and late phase clinical trials of Alzheimer's Disease (AD). Key uses of imaging include:
- MRI
- Eligibility Reads
- Safety Reads, including ARIA-E & ARIA-H
- Quantitative measures for efficacy endpoints (e.g. volumetric MRI)
- PET
- Eligibility & Study Population Enrichment
- Quantitative measures for efficacy endpoints (e.g. SUVR, brain extent)
The successful use of neuroimaging in clinical trials of AD requires the seamless combination of rigorous study operations, radiologic reads with robust data tracking, and state-of-the-art, validated image processing & analysis software to derive quantitative measures from high-quality images.
Imaging Biomarkers for Alzheimer's Disease
-
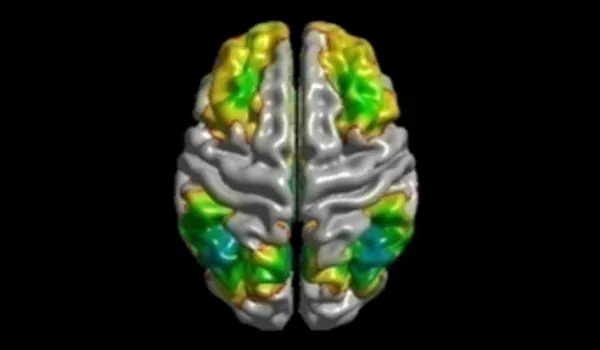
- Volumetric MRI (regional volumes & cortical thickness)
- Amyloid PET
- Tau PET
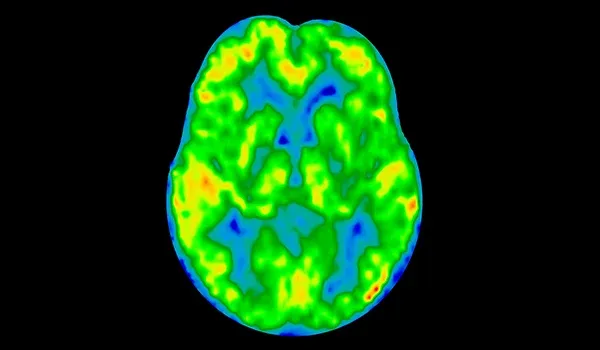
- FDG PET
- ASL Perfusion MRI
- fMRI (resting-state and task-based)
- Diffusion Imaging (e.g. DTI, NODDI, free water imaging)
Highlights from Our Alzheimer's Disease Imaging Research
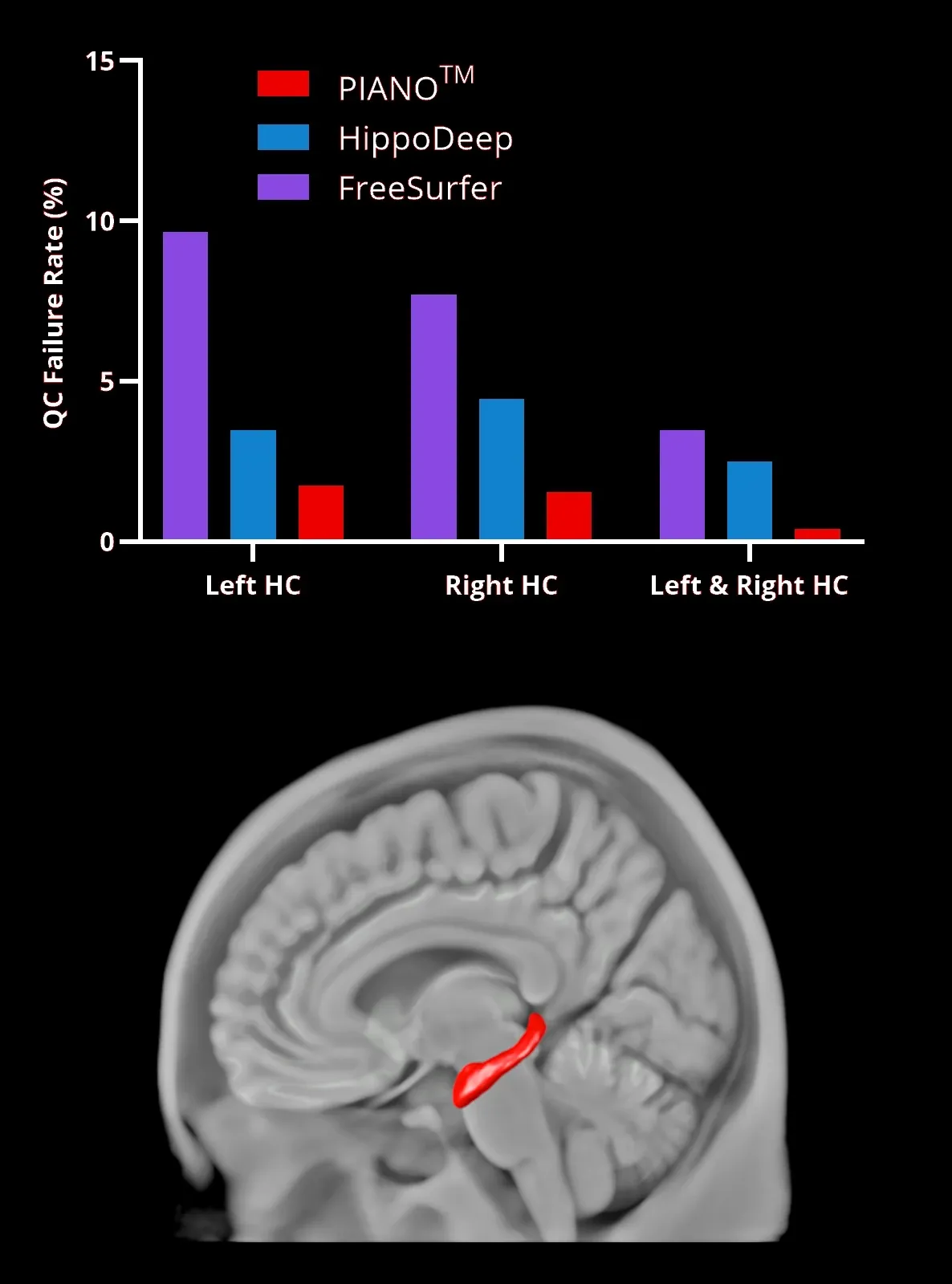
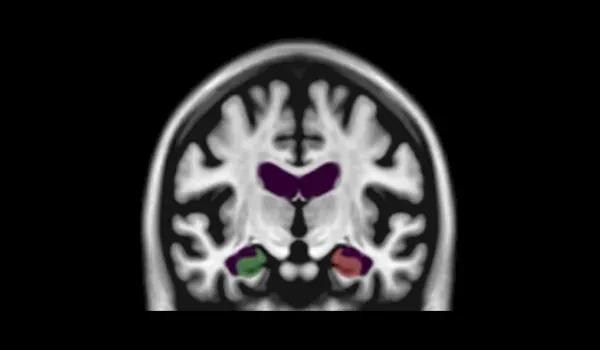
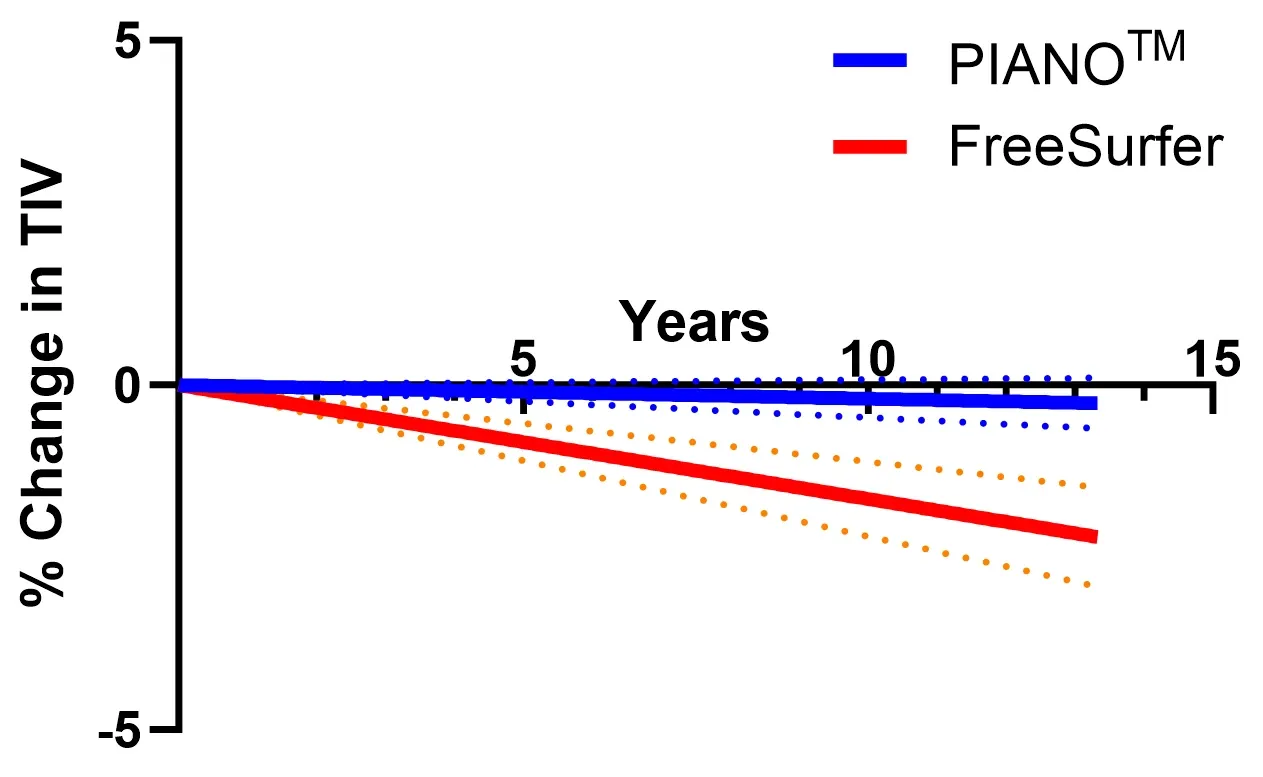
Hippocampus (HC, red region rendered in 3D) segmentation failure rates using PIANO™, HippoDeep, and FreeSurfer segmentation methods. Left & Right HC represents the case when the segmentation of both sides simultaneously fails in the same dataset.
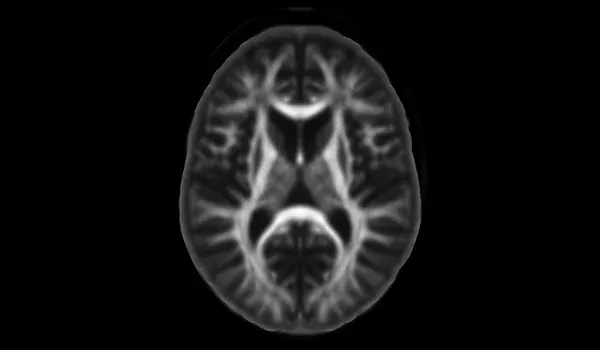
Deep Learning for Robust Segmentation of Hippocampus on MR Images
Deep learning models, particularly convolutional neural networks (CNNs), have revolutionized biomedical image processing by mimicking the human brain's feature identification process. U-Net architectures, with their encoder-decoder structures, have advanced neuroimaging applications, including region-of-interest (ROI) segmentation, by effectively training on smaller datasets augmented with realistic deformations (Kruger et al., 2013; Lindsay, 2021; Ronneberger et al., 2015).
Our work is focused on hippocampal segmentation, a challenging task due to this region's variability, especially in Alzheimer's disease (AD). Using a curated dataset of MRI scans, we have trained a U-Net model with labeled data, enriched by quality control and augmented training data. This method improves segmentation accuracy for challenging cases, such as hippocampal atrophy, where previous models failed (Thyreau et al., 2018).
Our deep learning model outperforms existing methods, such as FreeSurfer and HippoDeep, achieving a quality failure rate under 2% for either hemisphere and <0.4% for both hemispheres without manual corrections. This substantial reduction in quality control failure rate directly impacts clinical trial costs, as the lower data processing failure rate allows for potentially smaller trial sample sizes. This deep learning hippocampus segmentation was applied to an FTD dataset illustrating rapid early changes within the hippocampus.
In summary, our hippocampal segmentation deep learning model provides a reproducible, bias-free alternative to traditional methods, addressing challenges in neuroimaging with implications for broader ROI segmentation tasks.
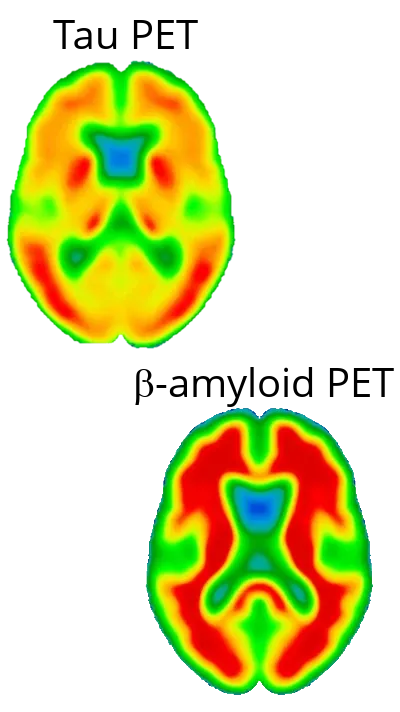
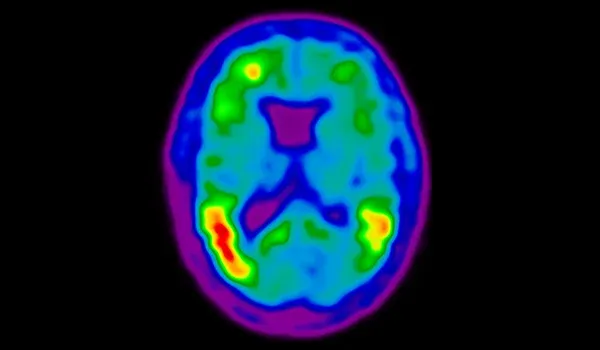
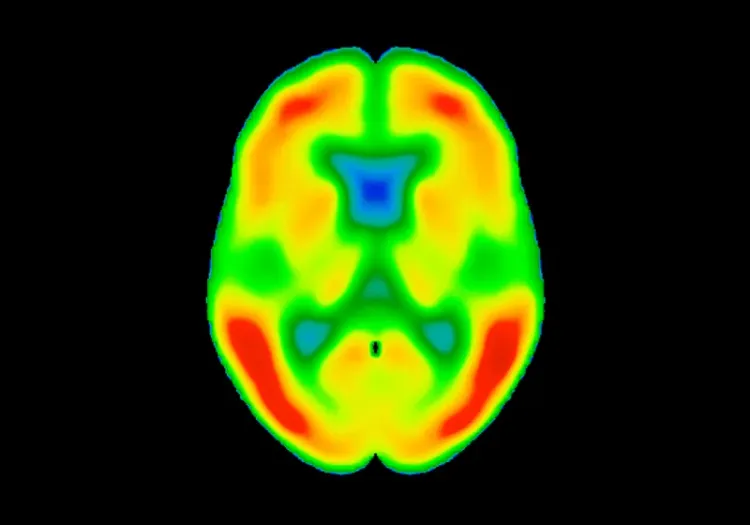
Neurodegeneration in AD is Primarily Driven by Tau, not Amyloid-β
Neurodegeneration in Alzheimer’s disease (AD) is increasingly recognized as being primarily driven by tau pathology, rather than amyloid-β (Aβ) deposition. While amyloid-β plaques have historically been seen as the hallmark of AD (Gouras, 2015), their presence does not strongly correlate with disease severity or neuronal loss (Gulisano, 2018). Instead, the accumulation of hyperphosphorylated tau protein in neurofibrillary tangles is more closely linked to the patterns of neuronal damage, cognitive decline, and disease progression (Liu, 2020; Moore, 2023). Tau pathology spreads in a regionally specific manner, often beginning in the entorhinal cortex and hippocampus before advancing to other cortical regions, aligning with the progression of clinical symptoms (Vogels, 2020). In our studies, spreading models and correlation analysis with cortical thickness as a measure of neurodegeneration strongly support the role of tau in driving neurodegeneration.
Further supporting this argument, therapeutic strategies that include targeting tau, such as tau aggregation inhibitors, anti-tau antibodies, and tau kinases, have shown promise in preclinical and early clinical trials (Congdon, 2023).
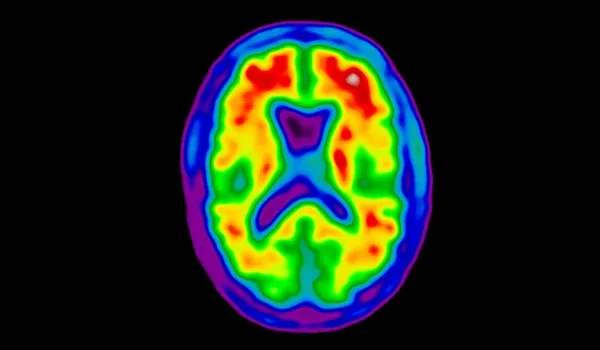
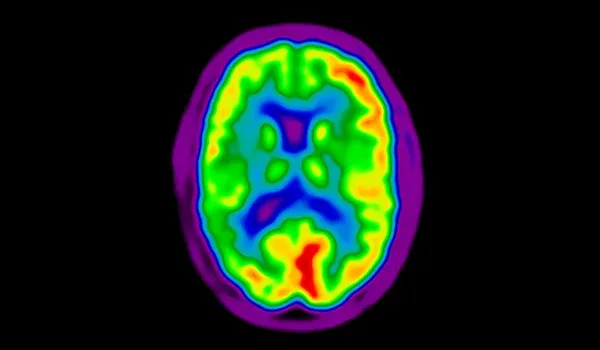
Raw PET image harmonized to the pre-defined common target resolution via computed smoothing kernel.
Harmonization of Spatial Resolution of PET Images in Clinical Trials without Phantoms
Biospective's SPITFIRE™ is an innovative computational method designed to harmonize brain positron emission tomography (PET) images across multi-center studies (Carbonell, 2024). Traditional approaches often rely on Hoffman phantom data to estimate spatial resolution (Joshi, 2009; Harrison, 2020), which can be limiting due to the unavailability of phantom images and potential sub-optimal results (Ruwanpathirana, 2024). SPITFIRE™ addresses these challenges by estimating spatial resolution directly from the PET images themselves, eliminating the need for surrogate phantom data. This method generalizes the logarithmic intensity plots technique to three dimensions, allowing for precise estimation of spatial resolution in both axial and in-plane directions. When applied to various cohorts, including different PET tracers and scanner models, SPITFIRE™ demonstrated consistent and reliable spatial resolution estimations, with minimal variability among subjects using the same scanner models and reconstruction parameters. This approach not only enhances the harmonization of PET images across different centers, but also provides a versatile framework applicable to a wide range of tracers and imaging modalities, such as SPECT.
Learn more about the use of neuroimaging in clinical trials of Alzheimer's Disease and our imaging biomarkers.
Discover more of our Therapeutic Areas
Related content
Up-to-date information on Alzheimer's Disease Imaging and best practices related to the evaluation of therapeutic agents in Alzheimer's Disease clinical trials.
Computational Method for Harmonization of Brain PET Images
A new algorithm for standardizing the spatial resolution of brain positron emission tomography (PET) images in multicenter clinical trials without phantoms.
Longitudinal Change in Tau PET in MCI & Alzheimer’s Disease
An overview of the natural history of change in Tau PET tracer uptake & binding in Mild Cognitive Impairment (MCI) & Alzheimer’s disease (AD).
Decreased Brain Glucose Metabolism in MCI is Driven by Tau
We demonstrate a more significant role of tau than β-amyloid in the reduction of cerebral glucose metabolism by analysis of PET images from the ADNI study.
Spatial Association of Amyloid & Tau Varies with Cognition
Using a computational approach, we found that β-amyloid & tau act in a spatially coordinated manner that depends on the cognitive stage of Alzheimer's disease.