Tauopathies & Rare Diseases Imaging in Clinical Trials Overview
Multi-modality imaging is widely used in early and late phase clinical trials of tauopathies (Progressive Supranuclear Palsy, Corticobasal Degeneration, Frontotemporal Dementia) and other rare diseases. Key uses of imaging include:
- MRI
- Eligibility Reads
- Safety Reads
- Quantitative measures for efficacy endpoints (e.g. volumetric MRI)
- PET
- Eligibility & Study Population Enrichment
- Quantitative measures for efficacy endpoints (e.g. SUVR, brain extent)
The successful use of neuroimaging in clinical trials of tauopathies & rare diseases requires the seamless combination of rigorous study operations, radiologic reads with robust data tracking, and state-of-the-art, validated image processing & analysis software to derive quantitative measures from high-quality images.
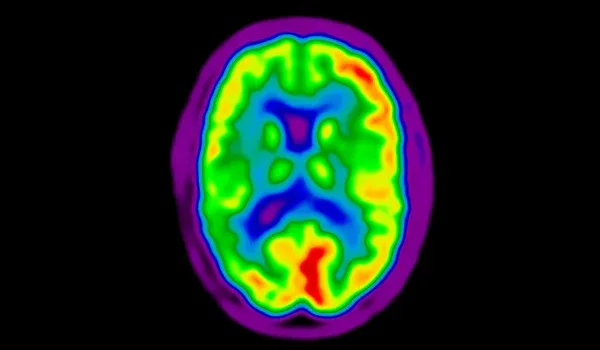
Imaging Biomarkers for Tauopathies & Rare Diseases
-
- Volumetric MRI (regional volumes & cortical thickness)
- Tau PET
- FDG PET
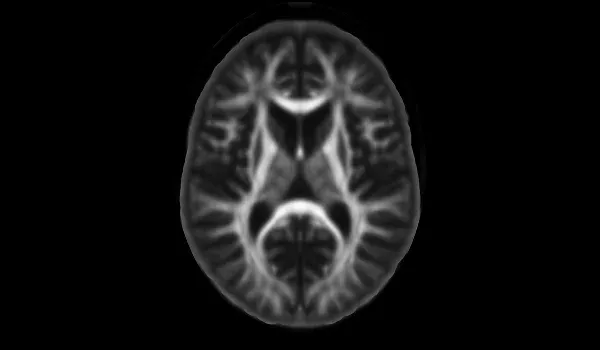
- Diffusion Imaging (e.g. DTI, NODDI, free water imaging)
Highlights from Our Tauopathies & Rare Diseases Imaging Research
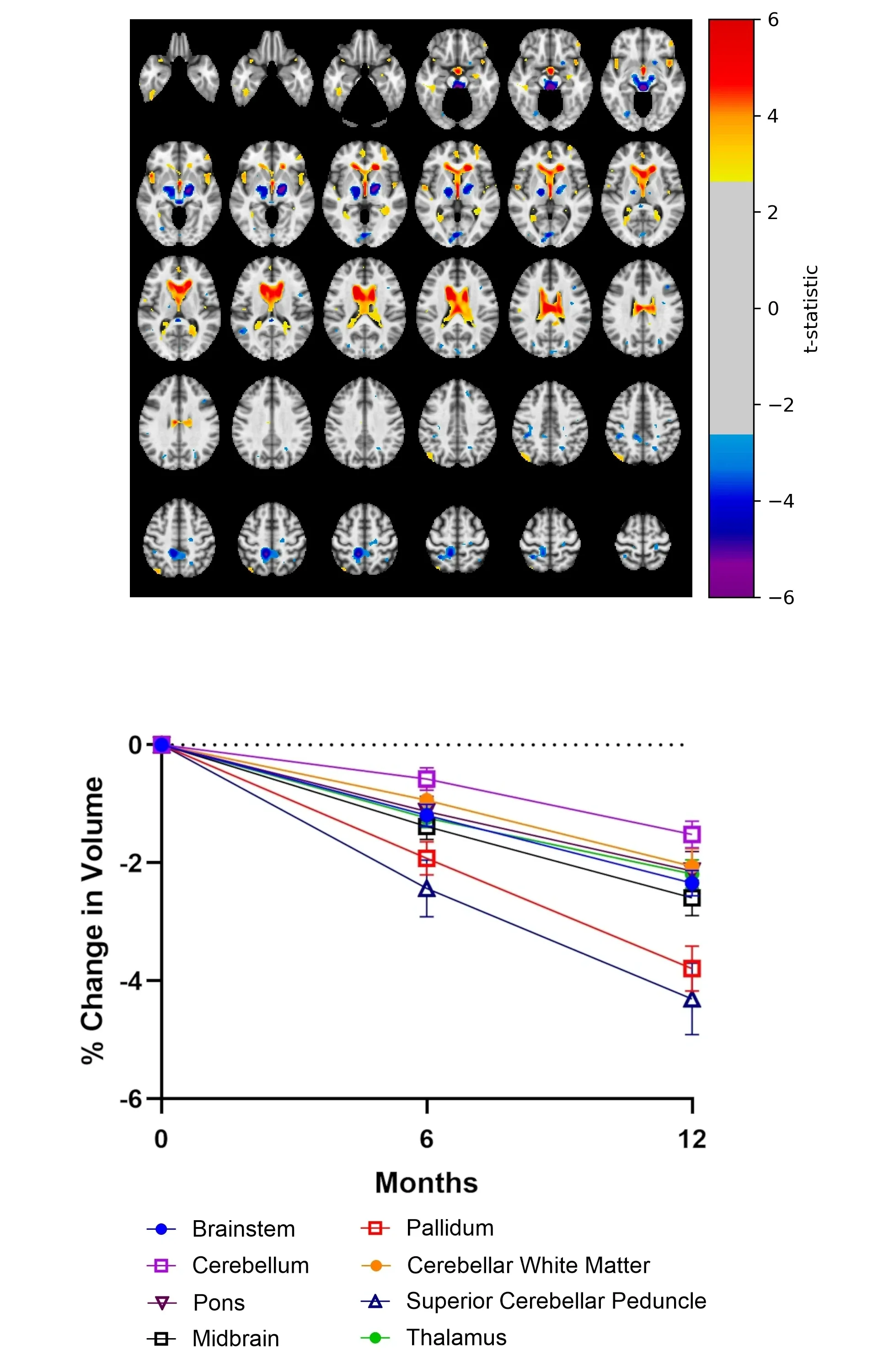
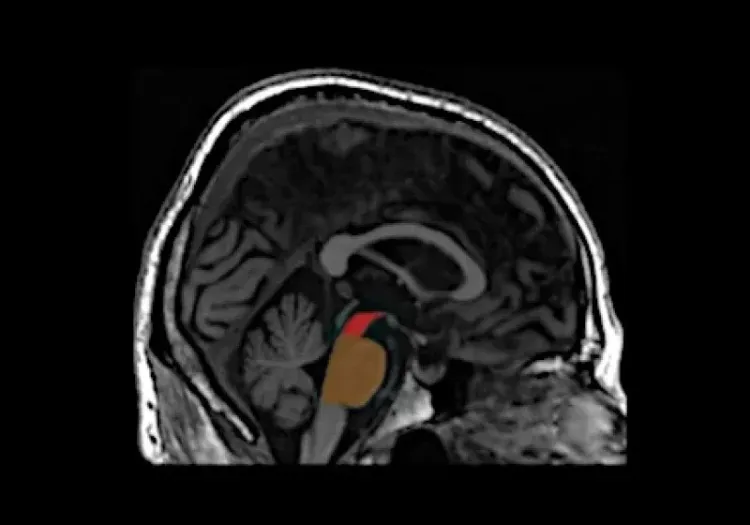
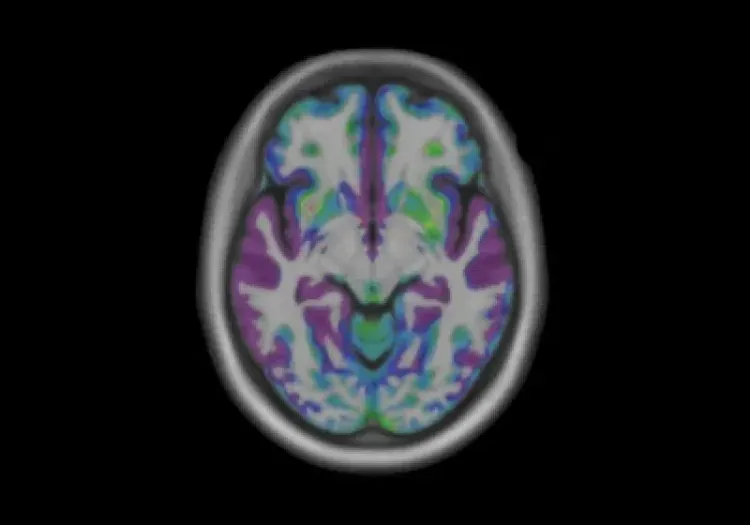
Top: Axial views of the t-statistic maps comparing the change in Jacobian determinants over a 12 month period in the Progressive Supranuclear Palsy group compared to control subjects highlighting the atrophy (blue to purple) throughout the cerebellum, pons, midbrain, and thalamus, along with the concurrent expansion of the ventricular spaces as well as the sulci adjacent to the insula region (yellow to red).
Bottom: The percent change in regional volumetric MRI data from baseline to 6 and 12 months in Progressive Supranuclear Palsy subjects.
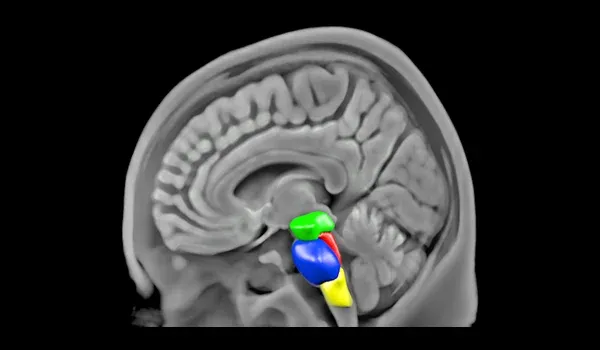
MRI Measures of Disease Progression for Progressive Supranuclear Palsy Clinical Trials
Progressive Supranuclear Palsy is a rare neurodegenerative disorder marked by movement, balance, speech, and eye movement difficulties. As an atypical Parkinsonian syndrome, Progressive Supranuclear Palsy is distinguished by tau protein accumulation leading to neuronal deterioration, particularly in the brainstem (Coughlin, 2020). Midbrain atrophy is a key disease hallmark, classically identified by radiological MRI-based features (Groschel, 2006; Page, 2020), structural changes in these regions can be quantified using planimetric measures such as the Magnetic Resonance Parkinsonism Index (MRPI) and MRPI 2.0 (Quattrone, 2018).
Using our automated image processing pipeline (PIANO™) to analyze Progressive Supranuclear Palsy imaging data from the 4-Repeat Tauopathy Neuroimaging Initiative (4RTNI), we aim to identify reliable neuroimaging biomarkers for early diagnosis and accelerate therapeutic evaluations in clinical trials.
MRI-based volumetric analysis shows significant, region-specific atrophy patterns, providing insights into disease progression. Compared to traditional MRI biomarkers, PIANO™ requires substantially smaller sample sizes, detecting changes as early as 6 months from baseline. These findings support the use of automated MRI analysis for early diagnosis and clinical trials, facilitating faster evaluation of disease-modifying therapies. By improving accuracy and efficiency, this approach enables more effective monitoring of disease progression and therapeutic response.
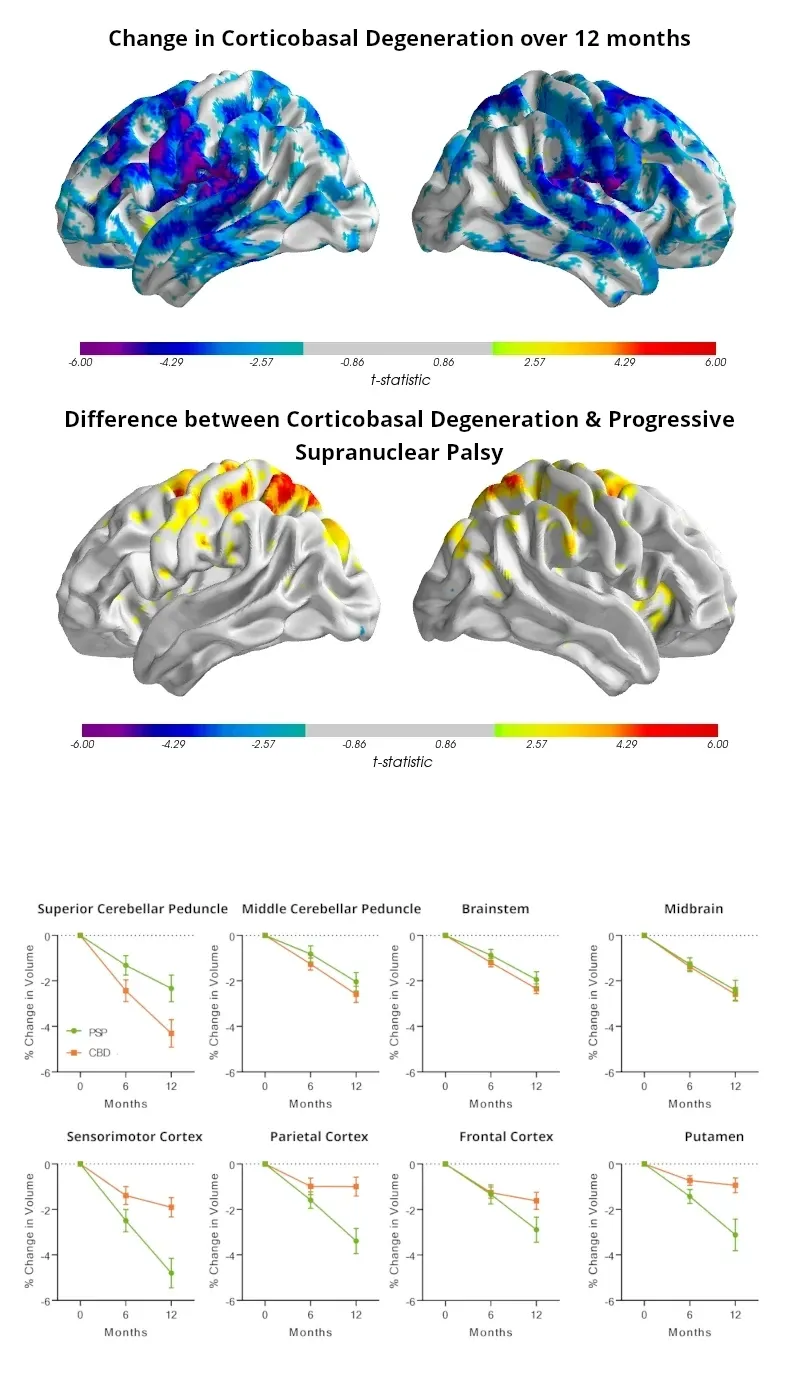
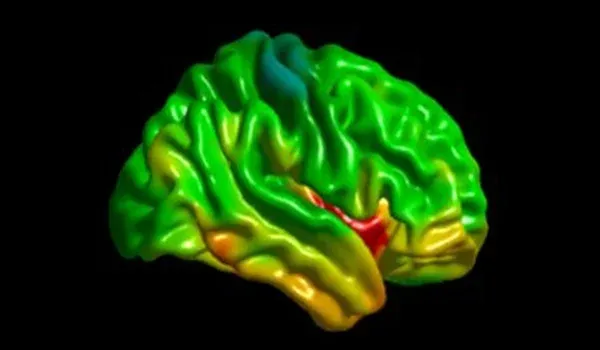
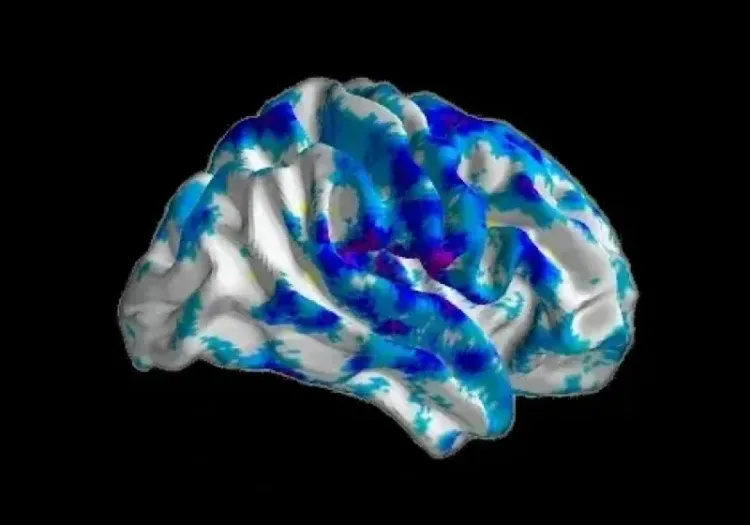
Top: Surface projections of the statistically significant (FDR-corrected, q=0.05) gray matter density change over time within the Corticobasal Degeneration population over a 12-month period, and the difference in gray matter density in the Progressive Supranuclear Palsy population compared to the Corticobasal Degeneration population at the 12 month time point.
Bottom: Percent change in regional volumetric data from baseline to 6 and 12 months are plotted for both the Corticobasal Degeneration (green) and Progressive Supranuclear Palsy (orange) subjects across a subset of the cortical and subcortical regions.
Automated MRI and Diffusion Imaging Biomarkers for Corticobasal Degeneration
Corticobasal Degeneration is a rare neurodegenerative disorder characterized by tau protein accumulation, leading to progressive motor and cognitive impairment. Symptoms include asymmetric motor disturbances, dystonia, apraxia, and alien limb syndrome, often overlapping with Progressive Supranuclear Palsy and Parkinson’s disease, making accurate diagnosis challenging. Pathologically, Progressive Supranuclear Palsy primarily affects the brainstem, while Corticobasal Degeneration shows more cortical involvement (Dickson, 2002). Neuroimaging biomarkers can aid in distinguishing these disorders, tracking disease progression, and evaluating treatment efficacy in clinical trials.
Using PIANO™, Biospective's automated image processing pipeline, we are assessing neuroimaging biomarkers in Corticobasal Degeneration subjects in the 4-Repeat Tauopathy Neuroimaging Initiative (4RTNI). Voxelwise and regional atrophy analysis reveal distinct disease-specific atrophy patterns: Progressive Supranuclear Palsy subjects show greater brainstem and cerebellar peduncle atrophy (2-4% over 12 months), while Corticobasal Degeneration subjects exhibit more cortical atrophy (3-5%).
Diffusion MRI changes in Corticobasal Degeneration subjects show rapid microstructural deterioration, particularly in parietal white matter and cortical regions. PIANO™-based volumetric analysis requires significantly smaller sample sizes (fewer than 50 subjects per arm) compared to FreeSurfer to detect a 60-80% reduction in disease progression.
These findings support automated analysis of anatomical MRI and diffusion imaging as promising biomarkers for early diagnosis and therapeutic evaluation in Corticobasal Degeneration clinical trials.
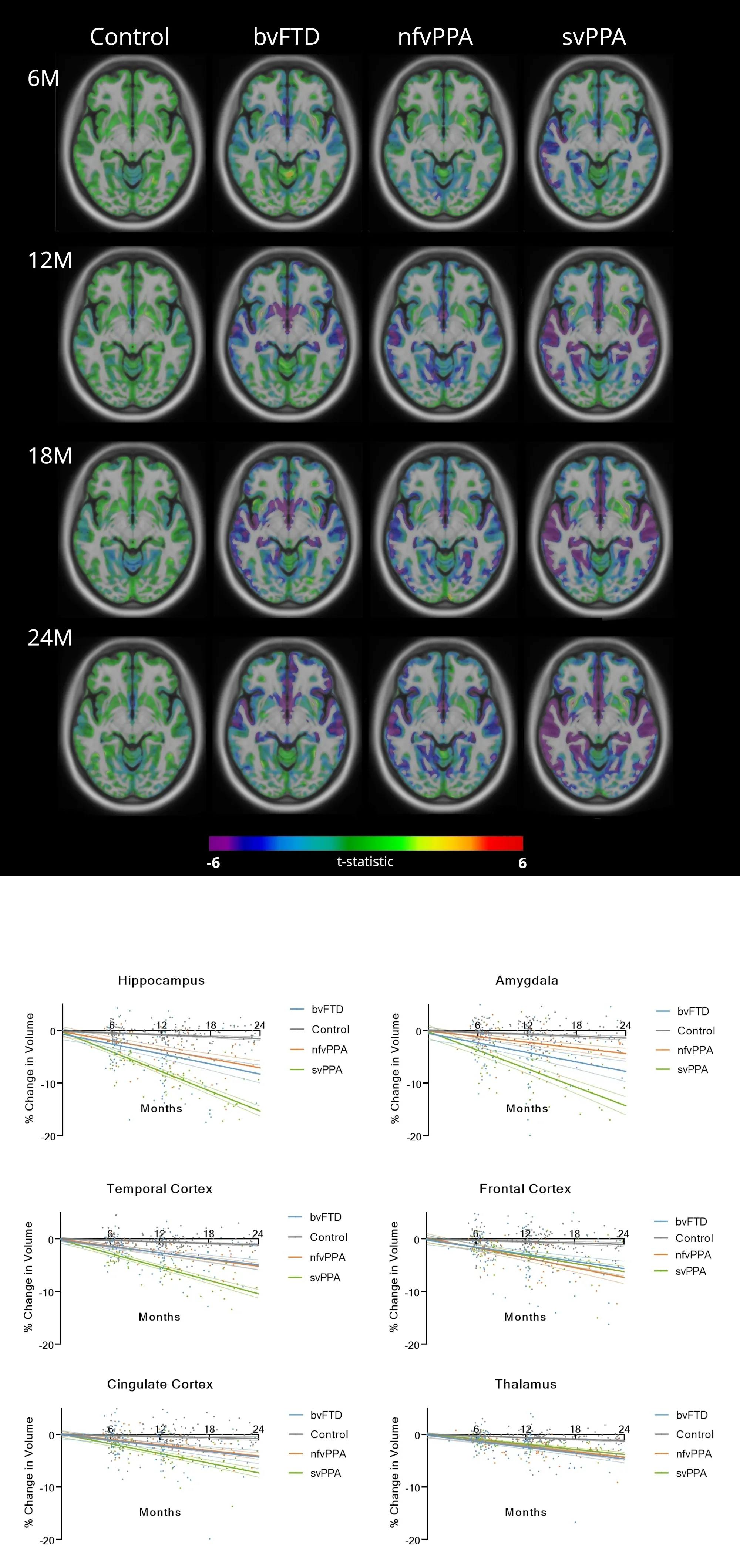
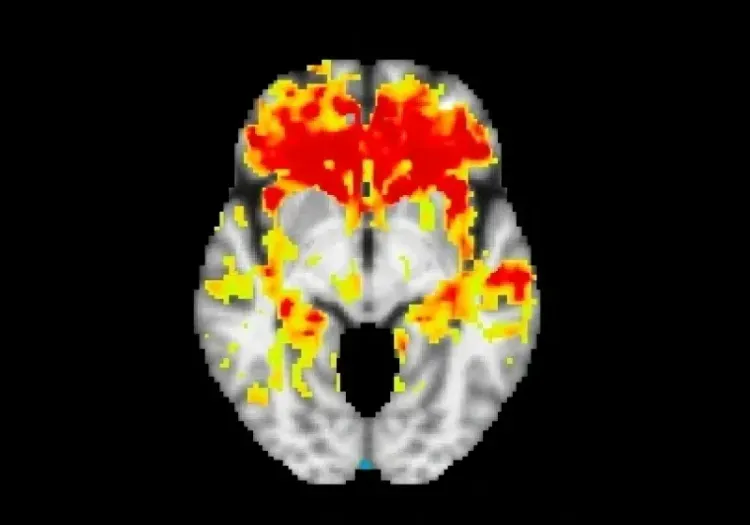
Top: The gray matter density t-statistic maps overlaid on an anatomical MRI template illustrate the statistically significant (FDR= 0.05) gray matter density change over time. The comparisons highlight the spatial (left to right) and temporal (top to bottom) variations in gray matter density changes comparing Control, bvFTD, nfvPPA, and svPPA populations over 6, 12, 18, and 24 months.
Bottom: The percent change in regional volumetric data from baseline to 24 months are plotted comparing the three FTD variants: bvFTD (blue), nfvPPA (orange), and svPPA (green), with healthy control subjects (gray) across a subset of the cortical and subcortical regions.
Automated MRI and Diffusion Imaging Biomarkers for Frontotemporal Dementia
Frontotemporal dementia (FTD) is a progressive, heterogeneous (clinical and pathologic) group of neurodegenerative disorders characterized by degeneration of the frontal and temporal lobes of the brain and progressive changes in behavior, language, and cognition. The three main clinical subtypes are behavioral variant FTD (bvFTD), non-fluent variant primary progressive aphasia (nfvPPA), and semantic variant primary progressive aphasia (svPPA).
Accurate diagnosis and monitoring of FTD variants, including behavioral variant FTD (bvFTD), non-fluent variant primary progressive aphasia (nfvPPA), and semantic variant primary progressive aphasia (svPPA) (Hogan, 2016; Leroy, 2021), remain challenging. Neuroimaging biomarkers can aid in differential diagnosis and assessment of disease progression.
We are utilizing PIANO™, Biospective's fully-automated image processing pipeline, to analyze MRI and diffusion MRI (dMRI) data from participants in the Frontotemporal Lobar Degeneration Neuroimaging Initiative (FTLDNI) database. Quantitative volumetric and diffusivity measures identify distinct spatial atrophy and microstructural changes across FTD subtypes.
Our Key Findings
- Anatomical MRI-derived atrophy measures effectively differentiate FTD variants.
- Diffusion MRI metrics, including diffusivity & free water, provide additional insights into microstructural degeneration.
- FTD subtypes exhibit distinct regional atrophy patterns, with bvFTD showing extensive frontal atrophy, nfvPPA affecting the inferior frontal gyrus, and svPPA impacting the anterior temporal lobes.
- PIANO™ requires significantly smaller sample sizes compared to traditional analysis methods, enabling early detection of structural changes and reducing clinical trial costs.
These findings support the use of automated MRI and diffusion imaging as reliable biomarkers for early diagnosis and therapeutic evaluation in FTD clinical trials. The approach facilitates efficient assessment of disease progression and potential treatment effects, making it a valuable tool for multi-center studies.
Learn more about the use of neuroimaging in clinical trials of Tauopathies and our imaging biomarkers.
Discover more of our Therapeutic Areas
Related Content
Up-to-date information on Tauopathies & Rare Diseases Imaging and best practices related to the evaluation of therapeutic agents in clinical trials.
MRI Measures of Disease Progression for PSP Clinical Trials
MRI biomarkers (including brain atrophy) from the 4RTNI and FTLDNI natural history studies of Progressive Supranuclear Palsy (PSP).
MRI & Corticobasal Degeneration (CBD)
Longitudinal MRI brain atrophy measures from the 4RTNI and FTLDNI studies including sample size calculations for clinical trials of Corticobasal Degeneration.
Frontotemporal Dementia (FTD) & MRI Brain Atrophy
Neuroimaging biomarkers (including MRI brain atrophy) from the FTLDNI natural history study of Frontotemporal Dementia (FTD).
Diffusion MRI & Frontotemporal Dementia (FTD)
Diffusion neuroimaging analysis from the FTLDNI natural history study of Frontotemporal Dementia (FTD).